Click for pdf: Approach to a child with a cough
General presentation
Background
Cough is a common indication of respiratory illness and is one of the more common symptoms of children seeking medical attention. Not only does it cause discomfort for the child, cough also elicits stress and sleepless nights for their parents. Before we dive into the clinical approach to cough, let us review the respiratory physiology of cough.
Physiology
Mechanics of coughing – three phases:
- Inspiratory phase: air inhalation lengthens the expiratory muscles (favourable length-tension relationship).
- Compressive phase: contraction of expiratory muscles against a closed glottis leads to an increase in intrathoracic pressure.
- Expiratory phase: opening of the glottis results in high expiratory flow and audible coughs. During this phase, the airway undergoes dynamic compression and the expulsion of air facilitates airway debris and secretions clearance.
Cough pathway
Each cough is elicited by the stimulation of the cough reflex arc. Cough receptors, which are afferent endings of the vagus nerve (cranial nerve X), are scattered in the airway mucosa and submucosa. Some of these receptors are mechanosensitive and some are chemosensitive. Mechanoreceptors are sensitive to touch or displacement and are located mainly in the proximal airway such as larynx and trachea. Chemoreceptors are sensitive to acid, heat, and capsaicin derivatives through the activation of type 1 vanilloid receptor (TRPV1) and are located mainly in the distal airways. The receptor locations are represented by red dots in Figure 1.
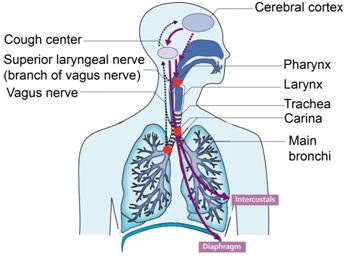
Figure 1 – Cough reflex anatomy: Red dots represent the locations of the cough receptors. Black arrows represent the afferent pathway and purple arrows represent the efferent pathway. (modified from Chung KF, Pavord ID. Prevalence, pathogenesis, and causes of chronic cough. Lancet. Apr 19 2008;371(9621):1364-74)
Via the vagus nerve, impulses from the cough receptors are propagated to the cough center in the medulla and nucleus tractus solitaris. Efferent impulses are generated from the cough centre and are propagated via the spinal motor (to expiratory muscles), phrenic (to the diaphragm), and vagus (to the larynx, trachea, and bronchi) nerves to the expiratory organs to produce cough (see Figure 1).
Classifications of Cough
Cough is usually classified based on its duration, quality or etiology. They are helpful indicators to guide your differential diagnosis. Note that these classifications are not mutually exclusive.
- Duration: acute (< 2 weeks), subacute (2-4 weeks), chronic (> 4 weeks)
- Quality: moist/wet/productive vs. dry
- Etiology: specific (attributable to an underlying problem) or non-specific (absence of identifiable problem)
Questions to ask
- Ask about the age/duration of onset (congenital cause).
- Nature of cough; How long has the child been coughing for?
- Acute/ subacute?
- Chronic paroxysmal cough?
- Chronic productive (wet-moist) cough?
- Barking/brassy sounding?
- Staccato sounding?
- Honking (Goose-like) sounding?
- Whooping sound?
- What time of the day is the cough worst?
- What type of exposure triggers the cough?
- What relieves the cough? Has the child been on medication before (ex. Bronchodilators)? Did this help with the present episode?
- Is there any shortness of breath (dyspnea)? Is there increased work of breathing?
- Is there associated vomiting (post-tussive emesis)? Is there hemoptysis?
- Is there evidence of fevers, failure to thrive or weight loss?
- Is the child passively or actively exposed to smoke from tobacco, marijuana, cocaine, or wood-burning stove?
- Ask about a history of choking (suspect foreign objects in airway).
- What pets or animals did the child have contact with?
- Ask about prenatal and neonatal history.
- Is there a family history of atopy (eczema, allergies, asthma), cystic fibrosis, and/or primary ciliary dyskinesia?
Differential diagnosis
| Duration | Common Etiologies |
| Acute cough(<2 weeks) |
|
| Subacute cough(2-4 weeks) |
|
| Chronic cough (> 4 weeks) |
|
Investigations
Physical Examination
- During the physical examination, you should pay attention to the following signs:
- ABC!
- Vital signs, including O2 saturation.
- Growth parameters – signs of poor growth and/or failure to thrive.
- Assess work of breathing.
- If patient able, listen to their cough.
- Inspect chest wall for signs of hyperinflation and deformities.
- General inspection for stigmata of chronic disease.
- Examine for nasal polyps and other nasal passage obstruction.
- Auscultate: is air entry symmetric? Are there adventitious sounds? Describe its location and quality (crackles, crepitations, wheeze)
- Auscultate for heart sounds.
- Examine for edema, cyanosis, clubbing of fingers/toes, and skin lesions.
Chest X-ray
- Chest radiograph can provide you with additional information, such as infiltrations/ consolidations, hyperinflation, peribronchial thickening, hyperinflation, atelectasis and chronic lung changes.
Pulmonary Function Test
- Can help delineate obstructive vs. restrictive lung disease
- Required in the diagnosis of asthma (child must be >6yo and cooperative)
Bronchoscopy
- Useful if suspicion for foreign body is high.
Mantoux Testing (Tuberculin Skin Test)
- To screen for tuberculosis infection.
References
- Chang AB. Pediatric cough: children are not miniature adults. Lung. 2010 Jan; 188 Suppl 1:S33-40.
- Chang AB, Glomb WB. Guidelines for evaluating chronic cough in pediatrics: ACCP evidence-based clinical practice guidelines. Chest. 2006 Jan; 129 (1 Suppl) :260S-283S.
- Chung KF, Pavord ID. Prevalence, pathogenesis, and causes of chronic cough. Lancet. Apr 19 2008;371(9621):1364-74
- Goldsobel AB, Chipps BE. Cough in the pediatric population. J Pediatr. 2010 Mar; 156 (3): 352-8.
- Grad R. Chronic cough in children. In: UpToDate, Mallory GB (Ed), Hoppin AG (Ed), UpToDate, Waltham, MA, 2009.
Acknowledgements
Writer: Calvin K.W. Tong
Edited by: Gaby Yang, Pediatric Resident


 (48 votes, average: 4.08 out of 5)
(48 votes, average: 4.08 out of 5)