Click for pdf: Basic Cardiac Physiology
Definition
The cardiac cycle, otherwise known as a “complete heartbeat”, involves the rhythmic muscular contractions of the heart through systole and diastole of both the atria and ventricles. Each phase of the cycle can be represented by waves on an electrocardiogram and consist of seven distinct phases:
| 1. Atrial Contraction | Fig. 1: The Cardiac Cycle – adapted from Williams and Wilkins, Cardiovascular Physiology Concepts 2005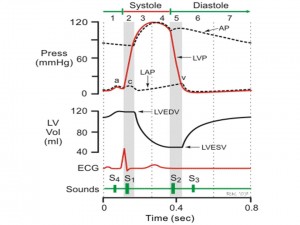 |
| 2. Isovolumetric Contraction | |
| 3. Rapid Ejection | |
| 4. Reduced Ejection | |
| 5. Isovolumetric Relaxation | |
| 6. Rapid Filling | |
| 7. Reduced Filling |
Systole consists of isovolumetric contraction and ventricular ejection (phases 2-4).
Diastole consists of isovolumetric relaxation and ventricular filling (phases 5-1).
General Presentation
Phase 1: Atrial Contraction
- Represented by the P-wave of the electrocardiogram, it is characterized by electrical depolarization of the atria. An AP fires at the SA node leading to atrial depolarization, which initiates contraction of the muscle of the atria and pressure within the atrial chambers consequently increases. This pressure increase then causes the atrioventricular valves (mitral and tricuspid valves) to open, forcing blood into the ventricles. Approximately 70 percent of blood goes into the ventricle and the remaining 30 percent is squeezed out through atrial contraction (P-wave).
- Following atrial contraction, the pressure of the atrial chamber begins to decline creating a pressure gradient forcing the atrioventricular valves to close. At this point in the cardiac cycle the ventricles are at end-diastolic volume (EDV) with the left ventricular end diastolic volume (LVEDV) at approximately 120 mL. This volume is known as the “preload” and is found to be at end diastolic pressures of 8-12 mmHg and 3-6 mmHg in the left and right ventricles respectively.
- The fourth heart sound, S4, an abnormal sound heard during atrial contraction, may be noticeable sound during this first phase of the cardiac cycle.
Phase 2: Isovolumetric Contraction
Represented by the QRS complex of the ECG, it is characterized by ventricular depolarization. The action potential has now arrived at the AV node, depolarizes the ventricles and initiates ventricular contraction.When ventricular pressure exceeds atrial pressure, the AV valves close which results in the first heart sound, S1, or the “lub”. After the AV valves close, the ventricular pressure rises rapidly as the ventricles are contracting against closed aortic and pulmonic valves. As there is no net movement of volume in or out of the ventricles, ventricular volume remains constant and contraction is said to be “isovolumetric”.” This indicates individual cardiac muscle fibres are lengthening and shortening through excitation-contraction coupling.
Phase 3: Rapid Ejection
- The moment intraventricular pressures exceed the pressure of the aorta and pulmonary artery, the aortic and pulmonic valves open. Blood ejects into the aorta and the pulmonary artery from the respective left and right ventricles. This results in a large decrease in ventricular volume and an increase in aortic pressure. At rest approximately 2/3 of the ventricle is ejected.
- No heart sounds should occur during this phase as the opening of the valves upon ejection of the blood is silent. If there is a sound then this may indicate a sign of valve disease or intracardiac shunts.
Phase 4: Reduced Ejection
- Almost immediately after ventricular contraction (approximately 200 msec), ventricular repolarization begins and is represented by the T-wave on the ECG. This causes a decrease in ventricular pressure and the rate of ejection declines.
- At the same time the left and right atrial pressures begin to return to an increased pressure slowly – due to a continuous venous return from the lungs through systemic circulation.
Phase 5: Isovolumetric Relaxation
- Once the aorta and pulmonary artery have exceeded the pressures of the ventricles the aortic and pulmonic valves abruptly close resulting in the second heart sound, S2 or the “dub”.
- After the valves have successfully closed the pressure in the aorta and pulmonary artery begin to rise and is then followed by a slow decline in resistance. The rate of this resistance is regulated by the relaxation of the muscle fibres by which is representative of the last phase of excitation-contraction coupling.
- At this time the ventricles are still decreasing in pressure, however the volume of blood remains the same as all valves to the ventricles are closed. This is known as the end-systolic volume and retains at approximately 50 mL in the left ventricle.
Phase 6: Rapid Filling
- During this phase the intraventricular pressures fall below the atrial pressures which results in the opening of the AV valves and subsequent diastolic ventricular filling. Even though blood is flowing into the ventricles, intraventricular pressure continues to decline because they have not yet reached a full relaxation state. Once the ventricles have reached a state of complete relaxation, the pressures begin to gradually rise as they fill with blood from the atria.
- A third heart sound, S3, which is found to be normal in children, may be noticeable during this phase.
- Phase 7: Reduced Filling
- In the final stage of the cardiac cycle the ventricles continue to be fill resulting in an increased pressure. As a result the pressure gradient across the atrioventricular valves is reduced and the rate of filling is decreased.
Cardiac Assessment technique:
In order to assess the various stages of the cardiac cycle it is important to understand the process of the cardiac cycle and how to enhance the noticeable sounds of the heart that indicate a proper functioning cardiovascular system.
Warm the stethoscope with hands
- Use the bell to hear low pitched sounds and the diaphragm to hear high pitched sounds.
- Auscultate with the patient in 3 positions:
- Lying on his or her back with the head of the bed raised at 30-45 degrees
- Sitting up
- Lying on his or her side
- Use a zig-zag pattern over the pericardium auscultating from the base to apex or apex to the base of the heart.
- Identify:
- S1 – The first heart sound (lub) can be heard the loudest at the mitral area. This sound represents the closure of the mitral and tricuspid valves and is a low pitched, dull sound at the beginning of ventricular systole.
- S2 – The second heart sound (dub). This is best heard at the base of the heart at the end of ventricular systole.
- When performing auscultation follow the sequence below for a proper cardiovascular assessment:
- Begin with the stethoscope at the second intercostals space along the right sternal border known as the aortic area in which blood travels from the left ventricle during systole through the aortic valve to the aortic arch.
- Move to the pulmonary area located at the second intercostals space along the left sternal border. This area represents blood that is being ejected from the right ventricle during systole, through the pulmonary valve to the main pulmonary artery.
- At the fifth intercostals space along the left sternal border which is the tricuspid area. This area involves the blood flowing from the right atrium through the tricuspid valve and filling the right ventricle during diastole.
- Finally, at the fifth intercostals space by the mid-clavicular line known as the mitral area. This area consists of blood flow through the mitral valve to the filling of the left ventricle during diastole.
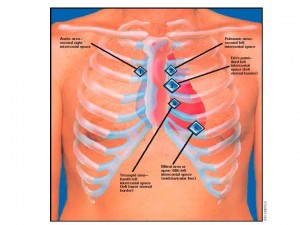
Fig. 2: Cardiac Assessment. Adapted from Seidel et al. 1995. Mosby’s guide to physical examination
Normal Heart Sounds of the Cardiac Cycle:
First Heart Sound – S1
- The first heart sound (“lub”) represents the closure of the mitral and tricuspid valves in early ventricular systole. You are mostly hearing the closure the mitral valve. It can be heard the loudest at the mitral area at the apex. However, if you want to listen specifically for the triscuspid valve, it is heard best at the left lower sternal border in the 4th intercostal space. This is a high frequency sound cause by vibrations of the valves and the walls of the heart, It isbest heard with the diaphragm of the stethoscope and is normally heard as a single sound.
Second Heart Sound – S2
- The second heart sound (“dub”) is produced by the closure of the aortic and pulmonic valves. It is also a high frequency sound. Pulmonic closure is best heard in the 2nd/3d intercostals space left sternal border and aortic closure is best heard in the 2nd/3rd intercostals space right sternal border.
- The individual components of S2, aortic (A2) and pulmonic (P2) vary with respect the respiration. During expiration, they are normally fused as one sound. Inspiration however, delays pulmonic closure and accentuates early aortic closure, a situation known as “normal” or physiological splitting of S2.
- This normal splitting can be explained by the decrease in negative intrathoracic pressure caused by inspiration. Negative intrathoracic pressure facilitates increased pulmonary capacitance (and reduces the impedance) of intrathoracic pulmonary vessels. Consequently, there is a temporary delay in the diastolic “back pressure” of the pulmonary artery responsible for the closure of the pulmonary valve. Thus P2 is delayed – it occurs LATER during inspiration than during expiration.
- Inspiration has the opposite effect on the aortic component because as the capacitance is increased with negative intrathoracic pressure, the venous return to the left atrium and ventricle transiently decreases. Reduced filling of the left ventricle leads to reduced stroke volume and thus the time required for left ventricular emptying is shortened. Consequently, A2 occurs EARLIER during inspiration than expiration.
Abnormalities in S2 can arise in the pattern of splitting:
| Widened Splitting | Fixed Splitting | Paradoxical Splitting | |
| Definition | Increased in the interval between A2 and P2; each component can be heard even during expiration and is more widely separated during inspiration | Abnormally widened interval between A2 and P2 that persists unchanged throughout respiration | “Reversed” splitting; the audible separation of A2 and P2 during expiration that disappears during inspiration |
| Mechanism | Delayed closure of the pulmonic valve | Chronic volume overload of R-sided circulation results in high capacitance, low-resistance pulmonary vascular system thus delaying the back pressure responsible for the closure of the pulmonic valve. Thus P2 occurs even later. | Abnormal delay in the closure of the aortic valve such that P2 preceeds A2 |
| Conditions Associated | Right bundle branch blockPulmonic stenosis | Atrial septal defect (ASD) | Left bundle branch blockSevere aortic stenosis |
Abnormal Heart Sounds of the Cardiac Cycle:
Extra Systolic Heart Sounds – Clicks:
- These sounds may occur in early, mid or late systole. Early extra systolic sounds include “ejection clicks” that occur shortly after S1. Clicks can be recognized as a high pitched heart sound and are best heard with the diaphragm of the stethoscope at the apex of the heart. Ejection clicks indicate the presence of aortic or pulmonic valve stenosis or dilatation of the pulmonic artery or aorta.. In stenosis, the sounds is associated with the abrupt deceleration when the valve reaches its elastic limit. In dilatation, the click is associated with sudden tensing of the aortic or pulmonic root with initiation of blood flow into the vessel.
- Systolic prolapse of the mitral or tricuspid valves often result in mid or late systolic clicks. They are caused by the chordae tendineae and mitral valve structures and occur when the mitral valve closes but a large cusp displaces into the left atrium. The click is usually present before a late systolic murmur caused by the regurgitation of a small amount of blood from the left ventricle into the left atrium.
Extra Diastolic Sounds:
- Extra sounds heard in diastole include the third heart sound (S3), the fourth heart sound (S4), the opening snap and the pericardial knock.
- Third Heart Sound – S3 – Ventricular Gallop:
- S3 is an abnormal heart sound that occurs at the end of the passive filling phase of either ventricle during early to mid diastole. It can best be heard as a dull, low pitched noise immediately following S2 due to tensing of the chordae tendinae during rapid filling and expansion of the ventricle. S3 can best be heard with the bell of the stethoscope with the patient in a supine or left lateral decubitus position. If it is heard at the tricuspid area then the right ventricle is faulty. If the sound occurs at the mitral area then the left ventricle is faulty. A pathological S3 can be referred to as a “ventricular gallop”. You can think of it in terms of a horse gallop which can be sounded out as: “Lub-Dub-By”.
- It is important to be aware that S3 can be a normal heart sound that occurs in children or young adults or even the last trimester of pregnancy. Here, an S3 represents the presence of a supple ventricle, capable of normal rapid expansion.
- In older adults, an S3 often indicates volume overload secondary to congestive heart failure or valvular regurgication.
Fourth Heart Sound – S4 – Pre-systolic Gallop:
- Another abnormal heart sound known as the “pre-systolic gallop” precedes S1 of the next cardiac cycle. It can be heard in late diastole and is caused by the vibration of the ventricular wall during atrial contraction characterized by the acceleration and deceleration of blood entering a chamber that resists additional filling. In other words, this sound is produced by the atrium forcefully contracting against a stiffened ventricle. It is also a dull, low pitched sound. You can sound it out as “Le-Lub-Dub” and can best be heard with the patient in supine position. Depending on which ventricle is faulty, you will have to listen for this sound in the tricuspid valve which would represent the right ventricle, and the mitral valve representing the left ventricle.
- The presence of S4 usually indicates cardiac disease secondary to a decrease in ventricular compliance caused by either ventricule hypertrophy or myocardial ischemia.
- S3 and S4: Both sounds can also be diagnosed, which is termed a “quadruple rhythm”in conjunction with S1 and S2. If a patient with both S3 and S4 develops tachycardia, diastole is shorted and the sounds become very close together in which they appear to be one sound. This situation is known as a “summation gallop”. This can be heard has a mid-diastolic, low pitched sound and can often be louder than S1 and S2.
Opening Snap
- An opening snap high pitched sounds that occur in early diastole as a result of mitral or tricuspid valvular stenosis, often secondary to rheumatic heart disease. It is a sharp sound that occurs shortly after S2 and does not vary much with respiration.
- A snap as a result of mitral stenosis (much more common than tricuspid stenosis) can be heard best with the diaphragm dial of the stethoscope between the apex and the lower left sternal border. An opening snap can sometimes be confused with a widely split S2 but with careful auscultation, 3 distinct sounds can be heard even in expiration. Snaps can be differentiated from S3 by the high pitch characteristic
Other Heart Sounds:
Rubs:
- A rub is a characterized as inflammation of the pericardium surrounding the heart and usually indicates pericarditis. It is represented by a scratchy, scraping, or high pitched screech that is usually louder during systole, but can occur in diastole or both.
- Place the diaphragm of the stethoscope at the third intercostals space along the lower left sternal border. Listen for a scraping or screeching by having the patient sit upright and lean forward while exhaling.
Appendix:
Diastole
- Referring to the time when the heart is in a period of relaxation and dilatation (expansion).
- End-diastolic Volume
- The amount of blood in the ventricle immediately before a cardiac contraction begins; a measurement of cardiac filling between beats, related to diastolic function.
Pericarditis
- An inflammation of the two layers of the thin, sac-like membrane that surrounds the heart. This membrane is called the pericardium, so the term pericarditis means inflammation of the pericardium.
P Wave
- A deflection in an electrocardiogram indicating depolarization of the atria.
- QRS Complex
- A group of waves depicted on an electrocardiogram; it actually consists of three distinct waves created by the passage of the cardiac electrical impulse through the ventricles and occurs at the beginning of each contraction of the ventricles. In a normal electrocardiogram the R wave is the most prominent of the three; the Q and S waves may be extremely weak and sometimes are absent.
Systole
- The blood pressure when the heart is contracting. It is specifically the maximum arterial pressure during contraction of the left ventricle of the heart. The time at which ventricular contraction occurs is called systole.
S1
- The heart sound that occurs with ventricular systole and is produced mainly by closure of the atrioventricular valves.
S2
- The heart sound that signifies the beginning of diastole and is caused by closure of the semi lunar valves.
S3
- The heart sound that occurs in early diastole and corresponds with the first phase of rapid ventricular filling.
S4
- The heart sound occurring in late diastole, corresponding with atrial contraction.
T Wave
- The first deflection in the electrocardiogram following the QRS complex, representing ventricular repolarization.
References:
1. Drury, N., and Gnanapragasam, J. 2005. Recurrent Noisy Pneumothorax Mimicking Pericarditis. International Journal of Cardiology, 113 (1): 104-105
2. Seidel, H. M., Ball, J. W., et al. 1995.. Mosby’s guide to physical examination (3rd ed.). St. Louis: Mosby-Year Book.
3. Springhouse, Williams L., and Wilkins. 2005. Professional Guide to Assessment. Lippincott Williams and Wilkins.
4. Williams L., and Wilkins. 2005. Cardiovascular Physiology Concepts. Lippincott Williams and Wilkins.
5. Lilly L.S. (Editor). Pathophysiology of Heart Disease 3rd Edition. Lippincott Williams and Wilkins, 2003.
Acknowledgements
Written by: John Hilhorst
Edited by Anne Marie Jekyll



 (22 votes, average: 3.77 out of 5, rated)
(22 votes, average: 3.77 out of 5, rated)
Hey,
What happened to your follow up article?
_______
Check out my Health article on Hipaa Laws
( http://community.sprint.com/baw/groups/sxsw-interactive/blog/2011/04/16/how-is-information-technology-helping-in-healthcare )