Background
Definition
Acne is an inflammatory condition of the pilosebaceous units, most often affecting the face and trunk, manifesting itself as comedones (comedonal acne), papulopustules (papulopustular acne) or nodules and cysts (nodulocystic acne and acne conglobata).
Acne is most common during the adolescent years. Though equally common in males and females it tends to be more severe in males, but more persistent (into mid-20s or even later) in females. 50% Of patients have a family history of acne. Pitted, depressed or hypertrophic scars may follow all types but especially nodulocystic acne and acne conglobata.
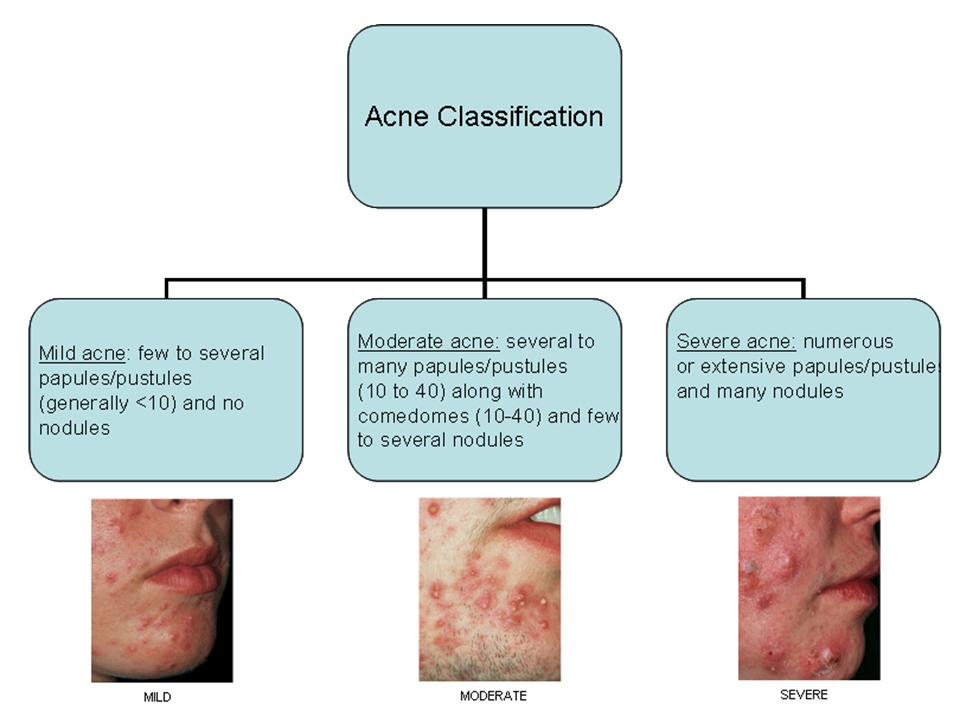
Some sources classify acne as inflammatory vs. non-inflammatory:
- Inflammatory acne – pustules and papules (<5mm) or nodules (>5mm)
- Non- inflammatory acne or comedonal acne – Primarily has open and closed comedones
Acne variants:
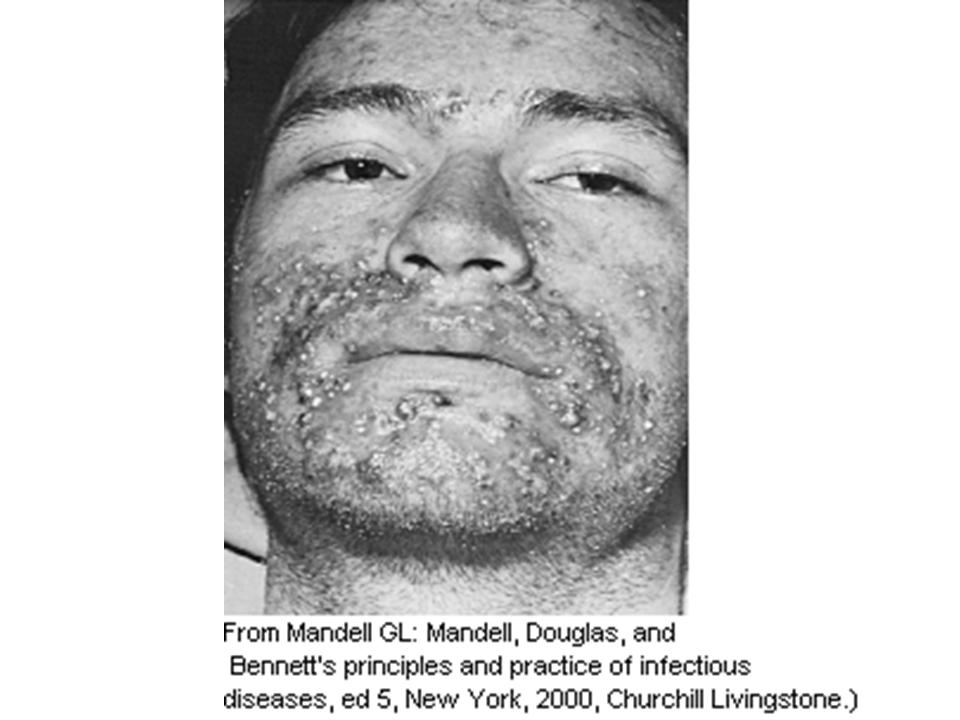
- Acne fulminans – an acute onset systemic condition associated with wide spread eruption of nodules and friable hemorrhagic plaques, together with fever and arthralgias.
- Acne conglobata – a severe form of nodular acne more common in males. Lesions are more prominent on the back, chest and buttocks. Large draining lesions, sinus tracts and severe scarring may occur.
Incidence and prevalence
Nearly 100% of adolescents are affected at one time or another, but only 15% seek medical advice. During adolescence adrenal maturation leads to proliferation of the pilosebaceous glands on the face and trunk, often resulting in the onset of acne. Acne however tends to resolve with age such that only 8% of individuals between the ages of 25 and 34 are affected, and only 3% of those between the ages of 35 and 44 year.
Pathogenesis
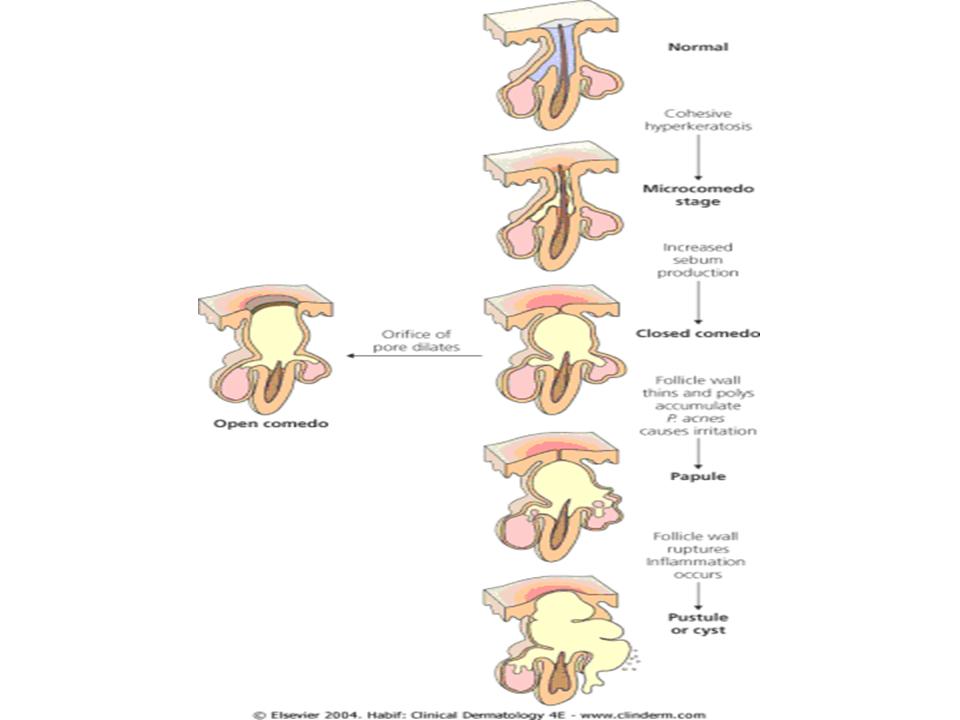
Acne results from a change in the keratinisation pattern in the pilosebaceous unit, with the keratinous material becoming denser and blocking the secretion of sebum. These keratin plugs are referred to as comedones.
The plugging of pilosebaceous units coupled with a complex interaction between androgens and bacteria in these plugged units leads to inflammation as follows:
- Overactivity/hyperresponsiveness of sebaceous glands occurs in response to androgens
- Colonization by Propionibacterium acnes, which metabolizes sebum to free fatty acid, and produces inflammatory mediators leading to inflammatory lesions
- The fatty acids and proinflammatory mediators cause a sterile inflammatory response to the pilosebaceous unit
- The distended follicle walls break and the contents enter the dermis, provoking an inflammatory and foreign body response. Rupture and intense inflammation are responsible for the scars
Questions to ask
Presenting condition
- Duration of lesions? How frequently do the lesions appear?
- Medications?
- Use of corticosteroids, anabolic steroids, isoniazid, lithium, phenytoin, and oral contraceptives with high androgenic activity may worsen acne
- Presence of other symptoms?
- If patient is generally well, acne fulminans (a rare variant of acne characterized by acute onset of severely inflamed lesions and accompanied by systemic signs and symptoms) is unlikely
- History of oligomenorrhea or hirsuitism?
- If present, these hormonal abnormalities may suggest acne caused by hyperandrogenism. Polycystic ovarian syndrome, late onset congenital adrenal hyperplasia or androgen secreting tumors should be considered
Contributory or predisposing factors
- Are there any acute or chronic stressors identifiable?
- Is there repeated occlusion and pressure on the skin such as by leaning face on hands or wearing helmets or chinstraps? (Acne mechanica)
- What type of cosmetics/hair products do you use? (Oil-based cosmetics and greasy hair products may contribute to acne)
Family history
- Do other members of your family have acne? (50% of patients have a positive family history.
Impact on emotional well-being
- How integrated is the individual in his community?
- What is his sense of self-worth?
- Are there any risks for self harm?
The psychological effect of suffering from acne can be profound. In rare cases embarrassment, anxiety and shame can lead to suicide. More commonly it leads to suboptimal functioning in social settings and employment.
Differential diagnosis
Comedones are required for the diagnosis of any type of acne and are NOT a feature of the conditions that follow
Rosacea
- Rosacea is a chronic facial skin disorder most commonly seen in individuals between the ages of 30 and 60 years of age. It is characterized by diffuse inflammation in center of face with telangiectasia, and erythematous papules, sebaceous hyperplasia and/or pustules. Unlike acne vulgaris, rosacea rarely occurs on the chest, back, shoulders, or scalp
Peri-oral dermatitis
- Characterized by small, grouped, erythematous papules in a perioral distribution. There is usually an unaffected rim of skin around the vermillion border.
Folliculitis
- Folliculitis is inflammation of hair follicles resulting from injury, infection, or irritation. It usually occurs as painful yellow pustules surrounded by erythema. A central hair is present in pustules and it can sometimes be associated with poorly chlorinated hot tubs (Pseudomonas folliculitis)
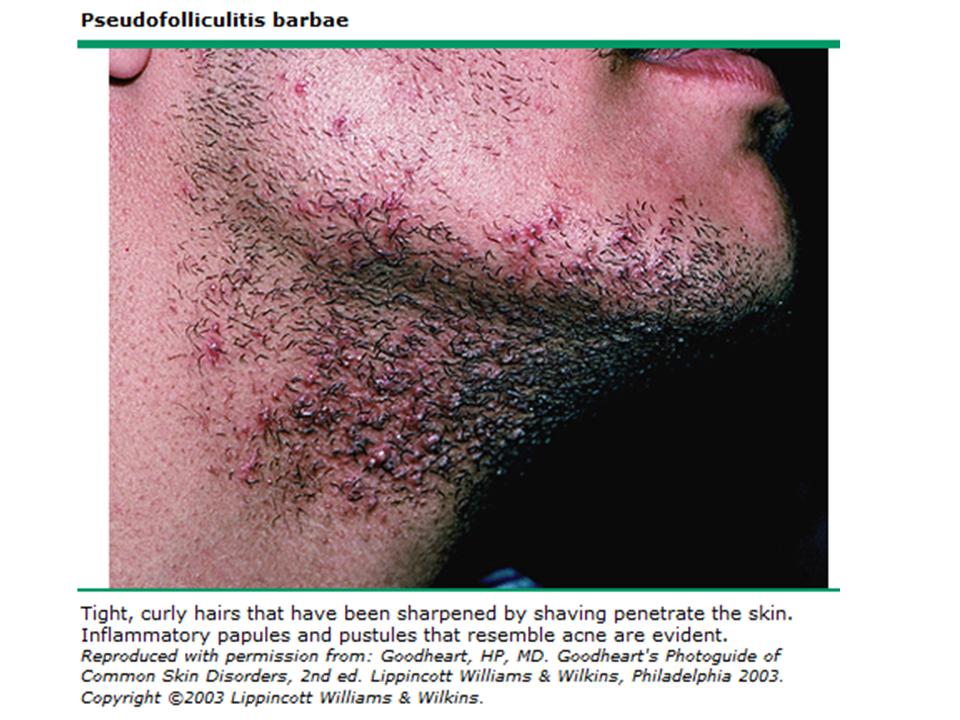
Pseudofolliculitis barbae
- Short shaved hairs curl back towards the skin, penetrate the skin and cause a foreighn-body inflammatory reaction. Inflammatory papules and pustules occur. The beard area is typically involved.
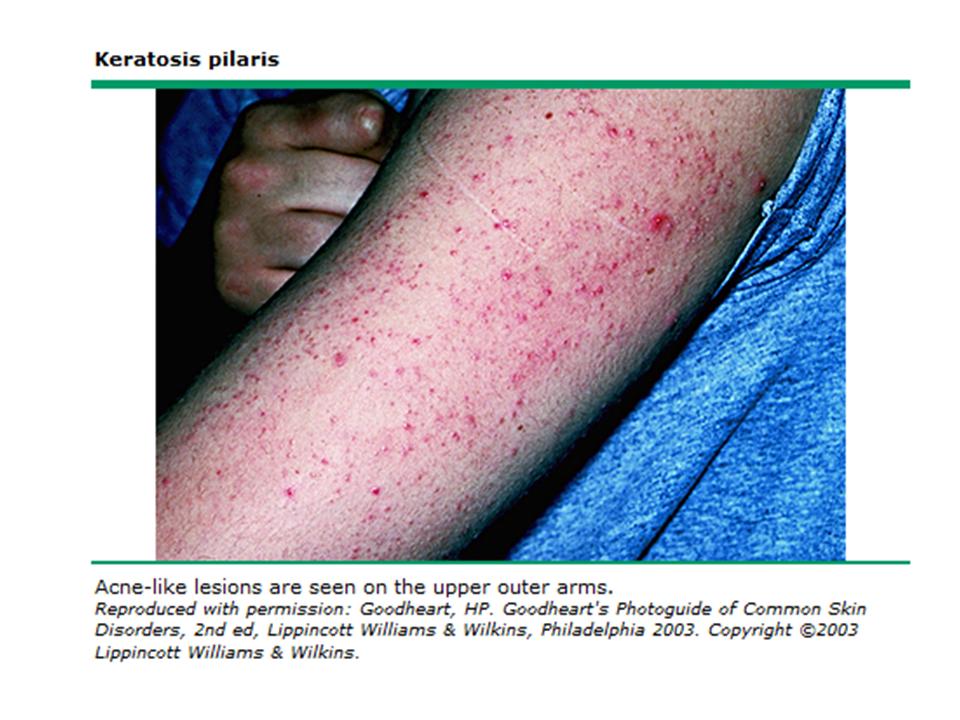
Keratosis Pilaris
- This is a common condition is caused by plugging of the hair follicles with keratin. It is mostly found on the extensor surfaces of the upper arms or thighs but can be found on the face.
Physical Examination
Examine the affected areas of skin, noting the type and number of lesions present. Treatment depends on acne classification.
Perform a general examination and measure the patient’s temperature in order to help distinguish between acne and cellulitis/folliculitis. Acute onset/worsening of acne coupled with fever and musculoskeletal symptoms may indicate acne fulminans
Investigations
Laboratory work is not routinely needed for most patients with acne.
Free testosterone, DHEAS, luteinizing hormone (LH) and follicle-stimulating hormone (FSH), and LH/FSH ratio are particularly useful in identifying PCOS as a cause of acne in females. 17-hydroxyprogesterone can be measured to screen for CAH
References
Habif, T. Acne, Rosacea, and Related Disorders in Clinical Dermatology : a color guide to diagnosis and therapy, 4th Ed (2004). Pages 162-194. Mosby, Edinburgh.
Usatine R, Pollack E and Baron E. Acne Vulgaris. FirstCONSULT, Copyright Elsevier 2007. http://www.firstconsult.com/fc_home/members/?urn=com.firstconsult/1/101/1014846
Wolff K, Johnson R and Suurmond, D. Disorders of Sebaceous and Apocrine Glands in Fitzpatrick’s Color Atlas and Synopsis of clinical Dermatology,5th Ed (2005). Pages2-14. McGraw-Hill.
Acknowledgements
Written by: Nicole Fernandes
Edited by: Elmine Statham





 (6 votes, average: 4.50 out of 5)
(6 votes, average: 4.50 out of 5)
Acne in teens.. Nifty 🙂