Click for pdf: Approach to Vomiting
Background
Vomiting is an organized, autonomic response that ultimately results in the forceful expulsion of gastric contents through the mouth.
Vomiting in children is most commonly acute infectious gastroenteritis; however, vomiting is a nonspecific symptom and may be initial presentation of serious medical conditions including infections (meningitis, septicemia, urinary tract infection); anatomical abnormalities (malrotation, obstruction, volvulus) and metabolic disease. Persistent and severe vomiting, if untreated, may result in clinically significant volume depletion and electrolyte disturbances.
Basic anatomy / physiology
Why / How does this occur in children?
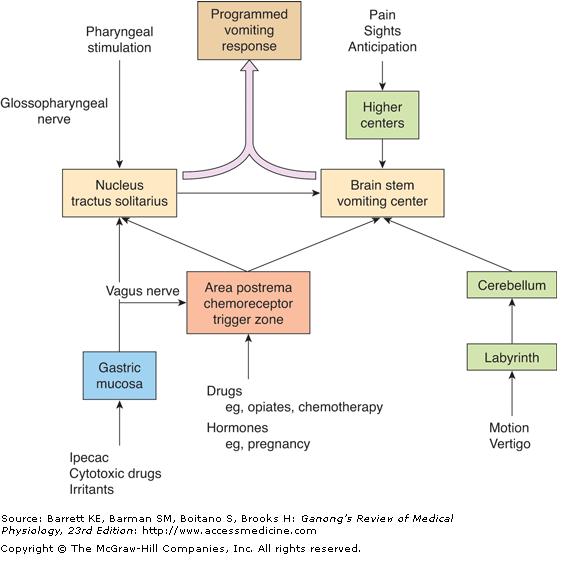
Vomiting is a coordinated autonomic response involving neural, hormonal, and muscular responses generated by the reticular formation of the medulla that consists of several scattered groups of neurons. The vomiting response may be triggered by peripheral and central stimuli (see figure 1). In particular, the area postrema in the medulla (unprotected by the blood brain barrier) samples peripheral blood and cerebrospinal fluid and likely causes vomiting associated with metabolic disorders and hormones.
Once the vomiting response is triggered, a pattern of somatic muscle action occurs with abdominal, thoracic, and diaphragm muscles contracting against a closed glottis. The resulting increased intra-abdominal pressure reverses the negative pressure of the esophagus and forces gastric contents upwards. The vomiting response also alters intestinal motility by generating a retroperistaltic contractile complex that moves intestinal contents towards the esophagus.
Classification
- Spitting up: small volumes (usually < 5-10 mL) of vomit during or shortly after feeding, often when being burped; typically caused by rapid/overfeeding and air swallowing
- Infant regurgitation: vomiting occurring ≥ 2 times per day for at least 3 weeks in the first 1-12 months of life in an otherwise healthy infant; often transient in nature and due to immature gastrointestinal tract
Central
- Vestibular – motion-sickness and vertigo
- Infectious – gastroenteritis, septicemia, non-GI infections
- Cortical – pain, strong emotions, smell, taste
- Drugs – chemotherapy, opiates
- Hormonal – pregnancy
- Metabolic – acidosis, uremia, hyperthyroidism, hypercalcemia, adrenal disorders
Peripheral
- Pharyngeal stimulation
- Gastric mucosal irritation
- Gastric and intestinal distension
History
History of Presenting Illness
- Characteristics of vomitus
- Smell
- Quantity
- Colour
- Blood – bright red/dark red/coffee-ground
- Bilious
- Timing
- Onset
- Duration
- Frequency
- Time of day
- Triggers
- Associated Symptoms
- Diarrhea
- Fever
- Abdominal pain/distension
- Anorexia
- Stool frequency
- Urinary Output
- Headache
- Vertigo
- Lethargy
- Stiff neck
- Cough
- Sore throat
Past medical history
- Chronic illnesses (diabetes)
- Travel history (infectious gastroenteritis)
- Sexual history (pregnancy)
- Ineffective use of birth control
- Last menstrual period
- Recent head trauma
- Toxin exposure
Medications
Allergies
Differential Diagnosis: Common causes of vomiting by age group
| Age | Acute | Chronic |
| Infant
1 month to 1 year |
Gastroenteritis
Pyloric stenosis Hirschsprung’s disease Acutely evolving surgical abdomen
Sepsis and non-GI infection Metabolic disorders |
Gastroesophageal reflux disease
Food intolerance Congenital atresias and stenosis Malrotation Intussusception |
| Children and adolescents | Gastroenteritis
Appendicitis Sepsis and non-GI infection Metabolic disorders Pregnancy Toxic ingestion |
Gastroesophageal reflux disease
Gastritis Food intolerance Cyclic vomiting Intracranial hypertension Inborn errors of metabolism Eating disorders |
Physical Exam Findings
Vitals
- Fever – sign of infection
- Hypotension, tachycardia – volume loss
Inspection
- Consciousness – intracranial hypertension, meningitis, metabolic disorders, toxic ingestion
- Weight loss – eating disorders, obstruction
Head and Neck
- Red, bulging tympanic membrane – ear infection
- Bulging anterior fontanelle and nuchal rigidity – meningitis
- Erythematous tonsils – upper respiratory tract infection
Cardiovascular system
- Tachycardia – infection, dehydration
Abdominal exam
- Abdominal distention – obstruction, mass, congenital abnormality, organomegaly
- Bowel sounds – high pitched tinkle (obstruction), absent (ileus)
- Guarding, rigidity, rebound tenderness – appendicitis, peritoneal inflammation
Skin and extremities
- Petechiae or purpura – serious infection
- Skin turgor, capillary refill – dehydration
- Jaundice – metabolic disorder
- Rashes – food intolerance, viral infection
Red flags: The following findings are of particular concern:
- Lethargy and listlessness
- Inconsolability and bulging fontanelle in an infant
- Nuchal rigidity, photophobia, and fever in an older child
- Peritoneal signs or abdominal distention (“surgical” abdomen)
- Persistent vomiting with poor growth or development
Procedure for Investigation (this will be based on the differential diagnosis)
| Condition | History and Physical | Diagnostic approach |
| Gastroenteritis | Diarrhea (usually), history of infectious contact, fever (sometimes) | Clinical evaluation |
| GERD | Fussiness after feeding, poor weight gain | Empiric trial of acid suppression |
| Pyloric stenosis | Recurrent projectile vomiting in neonates aged 3-6 weeks, emaciated and dehydrated | Ultrasound |
| Congenital atresia or stenosis | Abdominal distension, bilious emesis in first 24-48 hours of life | Abdominal X ray
Contrast enema |
| Malrotation | Bilious emesis, abdominal distention, abdominal pain, bloody stool | Abdominal X ray
Upper GI series with contrast under fluoroscopy |
| Sepsis | Fever, lethargy, tachycardia, tachypnea, widening pulse pressure, hypotension | CBC,
Cultures (blood, urine, CSF) |
| Food intolerance | Abdominal pain, urticarial, eczematous rash | Elimination diet |
| Metabolic disorders | Poor feeding, failure to thrive, hepatosplenomegaly, jaundice, dysmorphic features, developmental delays, unusual odors | Electrolytes, ammonia, liver function tests, BUN, creatinine, serum glucose, total and direct bilirubin, CBC, PT/PTT
Further specific tests based on findings |
| Non-GI infection | Fever, localized findings (sore throat, dysuria, flank pain) depending on source | Clinical evaluation
Further tests if needed |
| Serious infection | Meningitis
Pyelonephritis
|
CBC, Cultures (CSF, blood, urine) gram stains
CBC, Cultures (urine, blood) |
| Cyclic vomiting | At least 3 self-limited episodes of vomiting lasting 12 h, 7 days between episodes, no organic cause of vomiting | Diagnosis of exclusion |
| Intracranial hypertension | Nocturnal wakening, progressive recurrent headache made worse by coughing or Valsalva maneuver, nuchal rigidity, visual changes, weight loss, photophobia | Brain CT (without contrast) |
| Eating disorders | Body dysmorphism, teeth erosions, skin lesions on hand (Russell’s sign), binge eating behavior | Clinical evaluation |
| Pregnancy | Amenorrhea, morning sickness, breast tenderness, bloating, history of sexual activity and improper contraception use | Urine pregnancy test |
| Toxic ingestion | History of ingestion, findings vary depending on substance and pattern of ingestion | Varies depending on substance |
Conclusion
Vomiting is a symptom that can be caused by a variety of conditions that affect different organ systems. When evaluating a child with vomiting it is important to identify conditions in which immediate medical intervention is needed.
The most common causes of vomiting are age dependent and can cross over age ranges (see the above table for differential diagnosis based on age). If a child has prolonged vomiting (>12 hours in a neonate, >24 hours in children younger than two years of age, or >48 hours in older children) they should have appropriate investigations.
If a patient displays any of the following red flags, it is important to watch them carefully and have a low threshold for intervention:
- Lethargy and listlessness
- Inconsolability and bulging fontanelle in an infant
- Nuchal rigidity, photophobia, and fever in an older child
- Peritoneal signs or abdominal distention (“surgical” abdomen)
- Persistent vomiting with poor growth or development
References
(1) AccessMedicine | How to Cite Available at: http://www.accessmedicine.com.ezproxy.library.ubc.ca/citepopup.aspx?aid=5242514&citeType=1. Accessed 1/1/2011, 2011.
(2) Pediatric Care Online : Definition of Age Group Terminology Available at: http://www.pediatriccareonline.org/pco/ub/view/Pediatric-Drug-Lookup/153856/0/definition_of_age_group_terminology. Accessed 1/1/2011, 2011.
(3) Nausea and Vomiting In Infants and Children: Approach to the Care of Normal Infants and Children: Merck Manual Professional Available at: http://www.merckmanuals.com/professional/sec19/ch266/ch266l.html?qt=vomiting&alt=sh#sec19-ch266-ch266i-204f. Accessed 1/15/2011, 2011.
(4) Allen K. The vomiting child–what to do and when to consult Aust.Fam.Physician 2007 Sep;36(9):684-687.
(5) Scorza K, Williams A, Phillips JD, Shaw J. Evaluation of nausea and vomiting Am.Fam.Physician 2007 Jul 1;76(1):76-84.
Acknowledgements
Writer: Bing Wei Wang
Edited: Dianna Louie


 (40 votes, average: 4.55 out of 5)
(40 votes, average: 4.55 out of 5)