Click for pdf: Afebrile seizures
Background
Seizures are the clinical manifestation of aberrant, abnormal electrical activity in the cortical neurons. Thus they can be regarded as a symptom of cerebral pathology and are not in themselves a disease. The term epilepsy is not synonymous with seizures. Epilepsy, which comes from the Greek epilepsia meaning “taking hold of”, is a chronic disorder characterized by the tendency for spontaneous, recurrent seizures and requires at least two unprovoked seizures to be considered as a diagnosis.
Seizures occur in 3% to 5% of all children, making it the most common neurological disorder of the pediatric population. Febrile seizures occur in 2% to 4% of the pediatric population whereas epilepsy occurs in approximately 1%.
Questions to ask
- It is important to get a detailed account of the event or spell from a witness in order to answer the three questions above (Was the spell in question a seizure? What type of seizure? Cause of seizure?).
- Start with asking the witness to describe the spell from beginning to end. Then ask focused questions to ascertain details. Questions regarding the possible seizure can be divided into pre-ictal, ictal, and post-ictal categories.
Pre-ictal
- Was there any warning before the spell? If so, what was the warning?
- Did the child complain of abdominal discomfort, fear or any other unpleasant sensations before the spell?
- What was the child doing before the spell?
- Was the child asleep or awake prior to the event?
- Was the child sleep deprived prior to the spell?
- Were there any triggers for the spell?
- Was the child well before the spell or was there a fever or illness?
Ictal
- Was the child responding during the spell or was consciousness impaired?
- Did the child remember anything that occurred during the spell?
- Were there any repetitive behaviors during the episode, such as lip smacking, pulling at clothing, and constant rubbing of objects.
- Did any body movements occur?
- Was there any perioral cyanosis?
- What was the child’s skin colour during the event?
- Did the patient lose continence during the spell?
- How long did the spell last?
- How many episodes has the child experienced?
- How often do the spells occur?
Post-ictal
- How did the patient feel after the spell?
- Did the child seem confused and tired after the spell?
- How long did it take for the child to get back to baseline condition?
- Did the child suffer from a headache after the spell?
Other questions to ask:
- Has the child ever had any seizures before? Febrile seizures?
- Ask about past medical history, developmental history and current medications to rule out a symptomatic seizure.
- Is there any family history of seizures?
Diagnosis
Clinical categories
The categorization of seizures is important for determining treatment and prognosis
In order to describe the seizure you need to answer two main questions:
- Is the seizure simple or complex?
- simple seizure – consciousness is completely intact
- complex seizure – consciousness is impaired
- Is the seizure partial or generalized?
Partial seizure – involves a focal area of the brain and therefore affects a specific portion of the body. The clinical presentation of the partial seizure at onset indicates the location of the epileptic focus in the brain.
Generalized seizure – affects the whole body and involves the entire cerebral cortex.
Below follows a description of the different clinical seizure categories:
| Partial Seizures | Simple Partial | Focal in onsetNo impairment of consciousnessUsually short lived, rarely longer than 10 to 20 secondsAssociated with either motor, somatosensory/special sensory, autonomic or psychic (dysphasic, dysmnesic, cognitive, affective, illusions, structured hallucinations) symptoms.
Characteristic EEG demonstrates unilateral spikes or sharp waves in anterior temporal region, but discharges may be bilateral or multifocal on occasion. |
| Complex Partial | Focal in onsetImpairment of consciousness either from onset or simple partial developing into complex partial seizure.Average duration of seizure is 1 to 2 minutes, which is significantly longer than simple partial or absence seizures.Aura common, signals seizure onset in 30% children, who typically complain of epigastric discomfort, fear, or an unpleasant feeling. Auras occur before impairment of consciousness.
Automatisms (stereotypical, repetitive behaviors) characteristic of complex partial seizures and present in 50% to 75% of cases. Automatisms occur after impairment of consciousness and include: lip smacking, picking or pulling at clothing, constant rubbing of objects, and walking. EEG usually shows sharp waves or spike discharges in the anterior temporal or frontal lobe, but may on occasion reveal multifocal spikes. |
|
| Partial with secondary generalization | Focal in onset but then spreads throughout cortex causing a generalized seizure. | |
| Generalized Seizures (all complex) | Absence seizures OrPetit mal(Fr.: small bad) |
Seizures typically start around age 5 to 6 years.Characterized by short (5 to 20 second) lapses in consciousness, speech or motor activity.No auraNo postictal drowsiness
Automatisms may be present during the seizure and usually involve eye blinking or lip smacking. Often provoked by hyperventilation for 3 to 4 minutes. EEG demonstrates 3 cycles per second generalized spike and wave activity. Atypical absence seizures may involve myoclonic movements of the face or body and may result in loss of body tone causing the patient to fall. Furthermore, the onset and cessation of the seizure may not be abrupt as in typical absence seizure. EEG in atypical absence seizures often reveals either 2 to 2.5 or 3.5 to 4.5 cycles per second generalize spike and wave activity. |
| Tonic-clonic seizures OrGrand mal(Fr.: big bad) |
Characterized by sudden loss of consciousness and tonic-clonic, tonic or clonic contractions.Tonic contraction is an intense, generalized muscle contraction.Clonic contractions are rhythmic, often symmetric muscle contractions.Tonic-clonic contractions start with a tonic contraction and then produce clonic contractions.
Perioral cyanosis may be present. Loss of bladder may occur. Seizure is often followed by 30 to 60 minute deep sleep and postictal headache. |
|
| Tonic seizures | Involve intense muscle contraction only. | |
| Clonic seizure | Involve rhythmic, often symmetric muscle contractions only. | |
| Myoclonic seizure | Myoclonus refers to the spasm of a muscle or a group of musclesThese seizures occur either in isolation or in connection with other seizure types.Clinically characterized by brief, repetitive, symmetric muscle contractions. | |
| Atonic seizures | Sudden loss of postural tone causes child to fall.May be difficult to differentiate from other seizure types |
Etiology
Seizures are either symptomatic or idiopathic.
Symptomatic seizures are caused by:
- CNS Infection
- Meningitis
- Encephalitis
- Abscess
- CNS Trauma
- Acute trauma
- Previous trauma may lead to scar tissue formation
- Cerebrovascular
- Infarction
- Hemorrhage
- Arteriovenous malformation
- Venous thrombosis
- Hypoxic
- Hypoxic ischemic encephalopathy
- Metabolic
- Hypoglycemia
- Electrolyte disturbances
- Inborn errors of metabolism
- Neurologic effects of systemic disease
- Toxic
- Drugs
- Drug withdrawal
- Alcohol
- Alcohol withdrawal
- Lead poisoning
- Tumour
- Congenital CNS malformations
- Cortical dysplasia
- Lissencephaly
- Neurocutaneous syndromes (e.g. tuberous sclerosis)
- Fever – febrile seizures are discussed elsewhere
Idiopathic seizures
Idiopathic seizures occur in the absence of any underlying CNS pathology. Patients with idiopathic seizures are thought to have an increased susceptibility for seizures yet have normal brain function. Approximately 50% of seizure disorders in children can be placed in a seizure syndrome with unknown etiology.
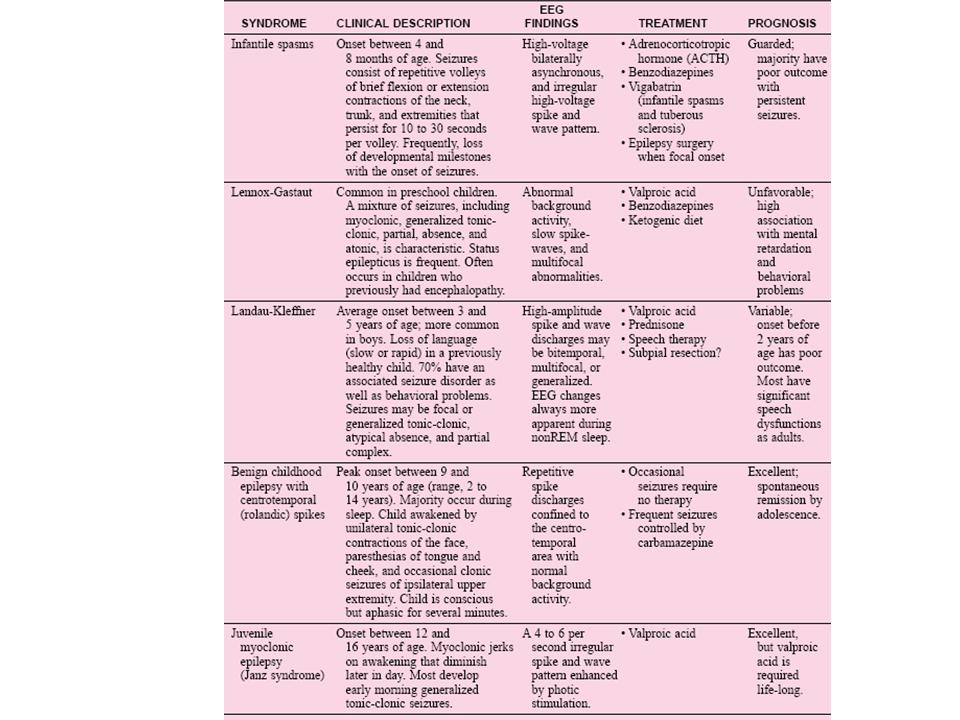
The details of all the seizure syndromes are beyond the scope of this paper. See Table I in appendix for a brief reference to five seizure syndromes found in children
Differential Diagnosis
Differential diagnosis for seizure includes:
- Syncope
- Breath holding spell
- Aspiration
- GERD
- Panic attack
- Daydreaming
- Conversion or pseudoseizures
- Benign sleep myoclonus
- Benign paroxysmal vertigo
- Complicated migraine
- Motor tics
- Complex behaviors
- Decorticate posturing
Physical Examination
All children who present with a possible seizure should have a complete pediatric exam.
Pay particular attention to the following elements of the physical exam:
- Vitals, including temperature
- Height, weight and head circumference – plot on a growth chart to determine percentiles
- Developmental stage of child in gross motor, fine motor, language and social domains. A delay indicates a cerebral insult. The insult may be remote (e.g. cerebral palsy), chronic ongoing (e.g. brain tumour), or may be secondary to another disease. Furthermore, developmental delay may occur in infantile spasms, an idiopathic epilepsy syndrome (See Table I).
- Signs of trauma. Direct trauma to the brain can be a cause or consequence of seizures.
- Signs of increased intracranial pressure
- Skin lesions – may suggest a neurocutaneous diseases underlying seizure activity. See the Table II in appendix for neurocutaneous disorders that can cause seizures in infancy.
Special tests:
- Fundoscopy – look for papilledema – suggests an increase in intracranial pressure (link to Signs of inc_ICP.doc).
- Neurologic exam – looking for focal deficits – indicates symptomatic seizure.
Include components:
- Mental status
- Cranial nerves
- Motor
- Reflexes
- Sensory
- Coordination and gait
- Brudzinski’s test and a Kernig’s test positive test suggest meningitis
Investigations
The particular investigations for each patient depend on the differential generated after the history and physical examination.
Blood tests
- In general, all patients should have acute symptomatic causes of seizures ruled out. Therefore all children should have the following tests perforemed:
- CBC and differential
- Electrolytes
- Calcium, phosphorus, magnesium
- Blood glucose level
Additional tests need to be considered when investigating the possibility of the following specific conditions:
- Hemorrhagic basis – INR, PTT
- Toxic basis – blood levels of suspected drugs and metabolites
- Genetic disease – possible karyotype and other tests specific to illness
Metabolic disease – tests specific to disease, may include:
- Ammonia
- Lactate
- Pyruvate
- Amino acids
- Urine organic acids
Lumbar puncture
- Lumbar puncture is indicated in:
- Infants <12months with a first time febrile seizure to rule out meningitis
- Infants 12 to 18 months with a simple febrile seizure
- Any child with meningeal signs
Imaging
- CT scan – indicated if head trauma is present/suspected
- MRI – indicated if the child has new or focal neurological deficits, recurrent seizures and/or papilledema
- EEG – children with their first seizure in the absence of fever (as recommended by the American Academy of Neurology). *** Note that many neurologists feel that this is unnecessary as EEG findings rarely impact treatment recommendations. Most offer EEGs more selectively when the seizure is focal, in a child < 1 year and associated with neurological abnormalities.
- Appendix
Table I: Summary of Five Seizure Syndromes found in Children (1)
Table II: Neurocutaneous Disorders Causing Seizures in Infancy (2)
References
Haslam, Robert H. A. Nonfebrile seizures. Pediatrics in review. 1997 Feb; 18(2): 40.
Fenichel, Gerald M. Clinical Pediatric Neurology, 3rd ed. Philadelphia: W.B. Saunders, 1997
Goetz, Christopher G. Textbook of Clinical Neurology, 2nd ed. Philadelphia : W.B. Saunders, 2003.
Hill, Alan. Neonatal Seizures. Pediatrics in Review. 2000 Apr; 21(4): 117-121.
Lindsay, Kenneth W. and Ian Bone. Neurology and Neurosurgery Illustrated, 4th ed. Philadelphia: Churchill Livingstone, 2004.
Polin, Richard A. and Mark F. Ditmar. Pediatric Secrets, 3rd ed. Philadelphia: Hanley and Belfus, 2001.
www.emedicine.com/neuro/topic527.htm (October 18, 2004) First Seizure: Pediatric Perspective. Author: Kenneth J. Mack, MD, PhD, Senior Associate Consultant, Department of Child and Adolescent Neurology, Mayo Clinic.
www.emedicine,com/neuro/topic415.htm (October 18, 2004) Seizures and Epilepsy: Overview and Classification. Author: Jose E. Cavazos, MD, PhD, Assistant Professor, Departments of Medicine, Pharmacology, University of Texas Health Science Center at San Antonio.
Acknowledgements
Written by: Sharan Mann
Edited by: Elmine Statham



 (51 votes, average: 4.59 out of 5)
(51 votes, average: 4.59 out of 5)