Click for pdf: Easy Bleeding
General Presentation
It is not uncommon for children to bleed and bruise after experiencing trauma. However, a child may also have an underlying coagulopathy, which results in easy and possibly life-threatening bleeding. It is key to distinguish between ‘normal’ and pathological bleeding.
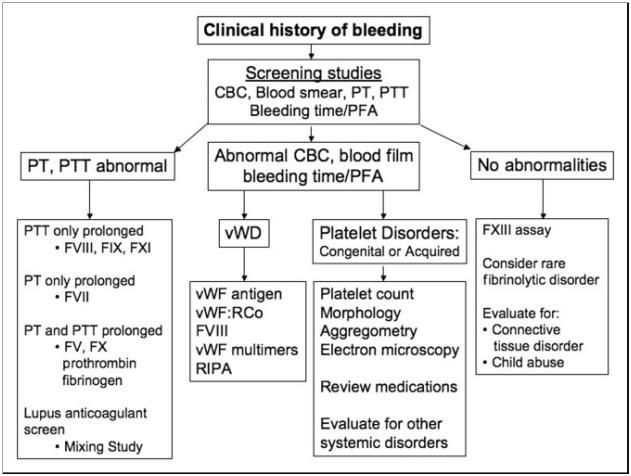
When dealing with clinically significant bleeding, it is important to have an approach to help focus your investigations (Figure 1). Bleeding may be the result of abnormalities in:
(1) Platelets
(2) Coagulation Factors
(3) Blood Vessels
Platelet Abnormality
Platelets are responsible for forming a plug that fills small defects in blood vessel walls that result from endothelial injury. This process begins immediately following injury. When platelets are either insufficient or dysfunctional, bleeding results. The bleeding that is associated with limited number or dysfunction of platelets involves the skin (i.e. petechiae, purpura, bruises, prolonged bleeding from superficial cuts) and mucus membranes (i.e. epistaxis, gingival bleeding, menorrhagia).
Coagulation Factor Abnormality
Coagulation factors are responsible for making a fibrin net to stabilize the platelet plug, and occlude larger vessel defects. This process occurs within minutes. When the coagulation factors are not being produced, or an inhibitor prevents their action, patients present with delayed bleeding in the form of large ecchymoses, hematomas, and hemarthroses.
Note that most coagulation factors are found as early as the 10th week of gestation in utero; however, their levels and activity only reach adult levels when children are 1 year old. Indeed, vitamin-K associated factors (II, VII, IX, X, protein C, protein S) are present in ½ normal adult values at birth, while fibrinogen, von Willebrand Factor, and factors V, VIII, XIII are often greater than adult values.
Vessel Abnormality
Vessels act as conduits for blood to move throughout the body. When their integrity is disrupted, one sees in non-hematological bleeding abnormalities, such as purpura, and bleeding within tissue parenchyma (lungs, nasal cavity, kidneys).
Assessment
A coagulopathy may be congenital or acquired, and a detailed clinical history will help guide the diagnostic process. It is thus crucial to inquire about the child’s history of bleeding and bruising, dating back to birth. A child with a congenital bleeding disorder will have a history of easy bleeding. A thorough history should include:
- History of bleeding and bruising, including epistaxis
- Bleeding with circumcision
- Bleeding with crawling/walking
- Bleeding with surgeries/sutures/dental interventions
- Menorrhagia – pad changes <2h, menses >7days, >1 menstrual period/month
- Prior transfusion requirements
- Family history of bleeding
- Medication use – prescription or accidental ingestion (i.e. ASA, Heparin, Warfarin)
- Recent illnesses
- A thorough review of systems
- Risk factors for non-accidental injury secondary to abuse
As with most presenting complaints in medicine, the second step in evaluating a clinical concern is a thorough physical examination. Key elements in the assessment of easy bleeding include:
- Detailed mucocutaneous exam for petechiae, purpura, ecchymoses, ulcers (skin, oropharynx, nasal cavity, perineum, ± gynecological exam)
- Hepatosplenomegaly
- Joint exam for range of motion and effusions
- If suspicious for non-accidental injury, assess for child’s motor developmental milestones
Once a thorough history and physical have been performed, investigations may be ordered in accordance with the clinician’s suspicions. All patients suspected of having a bleeding disorder should have a complete blood count, smear, as well as basic coagulation screen, including prothrombin time (PT) and its standardized measurement, the international normalized ratio (INR), as well as an activated Partial Thromboplastin Time (aPTT).
- PT: assess function of factors X, VII, V, II and fibrinogen (I)
- APTT: assess XII, XI, X, IX, VIII, V, II and fibrinogen (I)
- Thrombin Time: measure the formation of fibrin from fibrinogen
- Clotting Assay: to assess functional level of fibrinogen
- Platelet Count and Size: on complete blood count, confirmed on smear (particularly important if low #platelets on CBC as a smear will rule out the most common cause of “untrue thrombocytopenia”: platelet clumping)
- Bleeding time: assess vasoconstriction and platelet function
- Platelet Function Analyzer-100: assess platelet function
- Euglobin Lysis Time or fibrinogen: assess for accelerated fibrinolysis
Figure obtained from: Sharathkumar AA, Pipe SW. Pediatrics in Review. 2008; 29 (4): 121-130.
Etiology
The most common causes of bleeding disorders are acquired, due to hepatic dysfunction, vitamin K deficiency, disseminated intravascular coagulopathy, and, in children, immune/idiopathic thrombocytopenia purpura. The most common inherited disorder of easy bleeding is von Willebrand’s Disease. Note that the differential diagnosis for easy bleeding can be subdivided based on one’s approach to coagulopathy:
Platelet Abnormalities:
Quantitative-increased consumption/destruction/sequestration
- Medication induced (e.g.: heparin, GP IIb/IIIa inhibitors)
- Immune/idiopathic Thrombocytopenia Purpura
- Disseminated Intravascular Coagulation
- Thrombotic Thrombocytopenic Purpura
- Hemolytic Uremic Syndrome
- Hypersplenism (congestive, reactive, or infiltrative)
- HELLP
- Artificial heart valves or other foreign body
Quantitative-decreased production
- Medication induced (e.g.: antibiotics, valproic acid, antineoplastic agents)
- Infectious marrow suppression (e.g.: HBV, HCV, EBV, CMV, parvovirus, rubella, mumps, varicella, HIV)
- Nutritional (e.g.: lack of folate or vitamin B12, alcoholism)
- Marrow failure syndromes (i.e. Myelodysplastic Syndrome, Aplastic Anemia)
- Infiltrative (e.g.: leukemia, lymphoma, metastatic malignancy)
- Marrow replacement (e.g.:myelofibrosis, granulomas)
Qualitative
- Von Willdebrand’s Disease
- Drugs (e.g.: NSAIDs, antiepileptics such as valproic acid, antidepressants)
- Uremia, Liver Failure
- Congenital Heart Disease
- Bernard Soulier Syndrome (deficiency GP1b)
- Glanzmann Thrombasthenia (deficiency GPIIb/IIIa)
Factor Abnormalities
- Vitamin K deficiency (e.g.: nutritional, Cystic Fibrosis, Celiac Disease, biliary atresia, hemorrhagic disease of the newborn)
- Liver Failure (decreased hepatic synthesis, activation of coagulation and fibrinolysis ≈DIC, loss of proteins into ascites, vitamin K deficiency)
- Drugs (i.e. Heparin, Warfarin)
- Inhibitors – Auto-antibodies against clotting factors
- Factor VIII deficiency (Hemophilia A)
- Factor IX deficiency (Hemophilia B)
- Factor XI deficiency (Hemophilia C)
- Rare autosomal reccesive deficiencies in: factors V, VII, X, XI, XIII, fibrinogen
Vascular Abnormality
Hereditary
- Connective Tissue Disorders (e.g.: Ehlers-Danlos Syndrome)
- Osler-Weber-Rendu
Acquired
- Henoch-Schonlein Purpura
- Dysproteinemias
- Vitamin C deficiency (Scurvy)
- Cushing’s Syndrome
- Infections
- Medications
Management
Prompt and correct diagnosis of bleeding disorders is essential to initiate treatment, begin the referral process as indicated, and ultimately, to minimize patient morbidity and mortality. As is often the case in pediatric practice, teaching is required for the entire family regarding the condition and its possible treatments. Whenever possible, treatment should be aimed at correcting the underlying cause.
References
- Ambruso Daniel R, Hays Taru, Goldenberg Neil A, “Chapter 28. Hematologic Disorders” (Chapter). Hay WW, Jr., Levin MJ, Sondheimer JM, Deterding RR: CURRENT Diagnosis & Treatment: Pediatrics, 19e: http://www.accessmedicine.com/content.aspx?aID=3406649.
- Chi C, Pollard D, Tuddenham E.G., et Al. Menorrhagia in adolescents with inherited bleeding disorders. Journal of Pediatric and Adolescent Gynecology. 2010; 23 (4): 214-222.
- El-Bostany EA, Omer N, Salama EE, et Al. The spectrum of inherited bleeding disorders in pediatrics. Blood Coagulation & Fibrinolysis. 2008;19(8): 771-775.
- Ford, Jason. “Teaching Cases in Coagulopathy for Medical Students.” October 5, 2010, page 3.
- Konkle, BA. Acquired disorders of platelet function. Hematology – The Education Program of the American Society of Hematology. 2011; 2011: 391-396
- Malfait F, De Paepe A. Bleeding in the heritable connective tissue disorders: mechanisms, diagnosis, and treatment. Blood Rev. 2009; 23(5): 191-197.
- Sharathkumar AA, Pipe SW. Pediatrics in Review. 2008; 29(4): 121-130.
Acknowledgement
Writer: Lindsay McRae
Resident Editor: Katryn Paquette



 (3 votes, average: 4.33 out of 5)
(3 votes, average: 4.33 out of 5)