Click for pdf: Common pediatric bone diseases
General Presentation
Background: It is not uncommon for children to present with fractures after experiencing trauma. However, children may also present with pathological fractures, which are fractures that occur in abnormal bones and typically occur during routine activity or after minor trauma. It is important to be able to distinguish between traumatic fractures and pathological fractures as the prognosis and treatment can vary quite considerably. One also MUST consider non-accidental injury in the child that presents with multiple unexplained fractures. Non-accidental injuries are discussed in a separate article on this site.
These fractures will generally present as localized pain and tenderness over the involved bone. Refusal to weight bear in the younger, non-verbal child is also very common.
Pathophysiology: Although there are many potential etiologies for weakened bone manifesting as pathological fractures, it is simple to divide it into three categories with common etiologies:
1) Metabolic bone disease- eg. Rickets
2) Bone tumours – eg. Benign tumours (non-ossifying fibroma and osteochondroma) and malignant tumours (osteosarcoma and Ewing’s sarcoma)
3) Connective tissue bone disease- eg. Osteogenesis imperfecta
Metabolic Bone Disease: Normal bone growth and mineralization requires adequate calcium and phosphate. There are numerous etiologies of rickets, including nutritional deficiencies (calcium, phosphate and vitamin D), drug induced, renal pathology, and tumours. The end result and clinical manifestations of rickets are secondary to the failure of calcification of the growth plate cartilage because of a deficiency of either calcium or phosphate. Rickets is defined as deficient mineralization at the bone’s growth plate whereas osteomalacia refers to impaired mineralization of the bone matrix. Rickets is relatively common in children, especially those who have poor dietary intake, poor absorption, increased excretion of calcium, phosphate, or vitamin D, premature infants or breast-fed infants who are not supplemented with vitamin D. Regardless of whether it is calcium or phosphate deficient rickets, the typical clinical findings associated with Rickets include:
- Skeletal Findings(see Figure 1):
- Delayed closure of the fontanelle
- Parietal and frontal bossing
- Craniotabes (soft skull bones)
- Rachitic rosary (enlargement of the costochondral junction such that there is beading across the anterolateral aspects of the chest)
- Widening of the wrists; bowing the distal radius and ulna
- Progressive bowing of the femur and tibia
- Extraskeletal Findings(vary depending on the primary mineral deficiency):
- Calcipenic rickets – hypoplasia of dental enamel, decreased muscle tone, delayed achievement of motor milestones, hypocalcemic seizures, increased sweating
- Phosphopenic rickets – dental abscesses
Bone Tumors: Tumours, regardless of whether they are benign or malignant, can cause pathological fractures by growing and replacing the normal tissue of bone. This results in an abnormal, weakened bone more prone to fractures. In children, benign bone tumours are fairly common, but are often asymptomatic and discovered incidentally during evaluation for trauma or another condition, and thus, the true incidence is unknown. If they are symptomatic, they may present with localized pain, swelling, deformity or a pathological fracture. Most benign tumours generally present during the second decade. Two examples of common benign tumours which can present as pathological fractures include non-ossifying fibroma, and osteoid osteomas.
Malignant bone tumours account for 5% of all pediatric malignancies, with the peak occurrence between the ages of 10-24. The two most common malignant bone tumours in children are Ewing’s sarcoma and osteosarcoma which collectively make up 90% of the pediatric bone tumours. Ewing’s sarcoma is more common within the first 10 years, and then osteosarcoma becomes more common. The cancers often arise in the pelvis, femur, tibia and humerus. These can commonly present with symptoms of pain and swelling, which may be worse with exercise or at night, and sometimes the first signs may be due to a pathological fracture.
Connective Tissue Disease: Osteogenesis imperfecta (OI) is an inherited connective tissue disorder commonly known as “brittle bone disease” which can manifest in a wide spectrum, from mild to lethal forms. It is usually due to a deficiency of normal Type I collagen, which is an organic component necessary for proper bone formation. Although its incidence is estimated to approximately 0.005%, it is important to include this disease in the differential diagnosis because it can present early in children as numerous and recurrent pathological fractures. The common clinical manifestations of OI include:
- Multiple and/or atypical fractures
- Short stature
- Scoliosis
- Basilar skull deformities
- Wormian bones (irregular, small bones along the cranial sutures)
- Blue sclera
- Hearing loss
- Opalescent teeth that wear quickly
- Increased laxity of ligaments and skin
- Easy bruising
- Accelerated osteoporosis
Questions to Ask
- How did the fracture occur – How, when, where? – to determine if it was pathological or traumatic fracture
- Has the child had any previous fractures or any other concurrent fractures? If so, can you describe them? – to help determine pathological versus traumatic fracture
- What is the child’s diet like? To determine if nutritional deficiency Rickets may be the cause
- Did the child have any previous bone pain? If so, can you describe what makes it better or worse? Also, does it get worse at night? To check for potential bone tumors
- Does the child have a fever? To rule out any potential infectious causes or malignancies (constitutional symptoms – fevers, weight loss, drenching night sweats)
- Does the child have any other medical history? To rule out a secondary cause of the bone disease
- Do you suspect that the child may have been abused? Who is the primary caretaker of the child?
- Is the child taking any other medications?
Differential Diagnosis for Pathological Fracture
- Rickets from Vitamin D deficiency
- Osteogenesis Imperfecta
- Renal Osteodystrophy
- Osteomyelitis
- Child abuse
- Preterm birth resulting in osteopenia – neonates
- Fibrous dysplasia
- Osteomalacia
- Copper deficiency – infants: first 6 months
- Bone tumours and cancers
- Chronic Vitamin A toxicity
- Metabolic diseases – leading to calcium wasting and demineralization
- Prolonged administration of prostaglandins, glucocorticoids, or methotrexate
- Congenital syphilitic periostitis
- Hypophospatasia
- Juvenile Osteoporosis
Investigations and Management
1) Rickets:
Laboratory findings:
- Elevated alkaline phosphatase – indication of impaired bone mineralizeation
- Serum phosphorous concentrations – usually low in hypocalcemic and hypophosphatemic rickets
- Serum calcium concentration – decreased only in hypocalcemic rickets
- Parathyroid hormone – usually elevated in hypocalcemic rickets, but usually normal in hypophosphatemic rickets
- 25-OH Vitamin D – low in vitamin D deficiency
- GFR and Creatinine – to determine kidney function
Radiographic Findings:
- Osteopenia
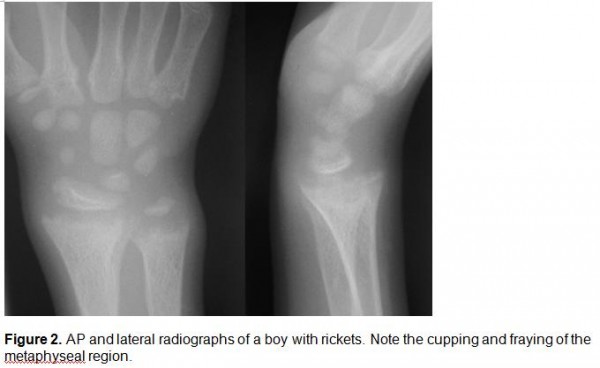
- Metaphyseal cupping and fraying (See Figure 2)
- Physeal widening
- Enlargement of costochondral junction
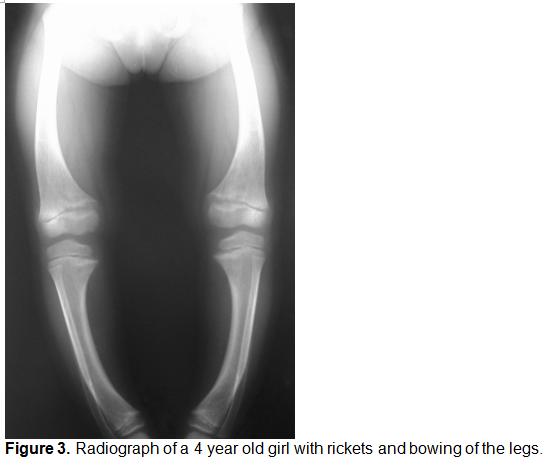
- Bowing of long bones (See Figure 3)
Management:
- Oral doses of 5,000-15,000 IU/day of Vitamin for 4 weeks for Vitamin deficient Rickets
- Optimize calcium intake for hypocalcemic rickets
- Treat underlying primary cause of Rickets
2) Bone Tumors (benign and malignant)
Laboratory Findings:
- If suspect malignancy: blood work including liver enzymes, CT chest, bone scan, bone biopsy, MRI of affected bone
Radiographic Findings:
- Benign: single lesion generally, sharp area of delineation, overlying cortex intact, sclerotic margins, no or simple periosteal reaction (See Figure 4)
- Malignant: multiple lesions often, poor delineation of lesion, loss of overlying cortex, extensive periosteal reaction, potential soft tissue involvement (See Figure 5)
Management:
- Benign: follow up with radiographs 4-6 months later
- Malignant: complete resection, chemotherapy, radiation
3) Osteogenesis Imperfecta
Laboratory Findings:
- Elevated levels of serum alkaline phosphatase
- Hypercalciuria – magnitude reflects severity of disease
- C-terminal peptide (marker of bone formation) and C-telopeptide (marker of bone resorption) –can be higher
Radiographic Findings:
- Mild OI: Thin cortex and relatively few fractures with normal skull development
- More severe OI: hyperplastic callus formation (from thickened periosteum), shortened long bones with multiple fractures (See see Figure 6)
Management:
- Bisphosphonates
Conclusion
Children who present with pathological fractures always require a thorough evaluation. It is important to keep an open mind as to the various causes of pathologic fractures and to always rule out non-accidental injury.
References
1) Beary J, Chines A. Clinical features and diagnosis of osteogenesis imperfecta. (Last Updated June 15, 2010) In: UpToDate, Tepas E (Ed), UpToDate, Wellesley, MA, 2010.
2) Scheri S. Differential diagnosis of the orthopedic manifestations of child abuse. (Last Updated Dec. 3, 2008) In: UpToDate, Wiley E (Ed), UpToDate, Wellesley, MA, 2010.
3) Rauch F. Overview of Rickets in Children. (Last Updated August 11, 2010). In: UpToDate, Hoppin A (Ed), UpToDate, Wellesley, MA, 2010.
4) Tis J. Overview of benign bone tumors in children and adolescents. (Last Updated September 28, 2010) In: UpToDate, Torchia, M (Ed), UpToDate, Wellesley, MA, 2010.
5) Kliegman R, Behrman, Jenson H, Stanton B. Nelson Textbook of Pediatrics, 18th ed. Philadelphia: Saunders, 2007.
6) Benson M, Fixsen J, Macnicol M. Children’s Orthopaedics and Fractures, 3rd ed. New York: Springer, 2010.
7) Kirpalani A, Babyn P. Imaging in Osteogenesis Imperfecta. eMedicine (Last Updated August 5, 2008). Available from http://emedicine.medscape.com/article/411919-print [Accessed on March 5, 2011]
8) Rijn R, McHugh K. Rickets Imaging. eMedicine (Last Updated March 18, 2009). Available from http://emedicine.medscape.com/article/412862-print [Accessed on March 5, 2011]
9) Dugani S, and Lam D. Toronto Notes. Toronto Notes Medical Publishing Inc. 2009
10) Jenny C. Evaluating Infants and Young Children with Multiple Fractures. Pediatrics. 2006; 118(3):1299-303.
11) Adam A, Dixon A. Adam: Grainger & Allison’s Diagnostic Radiology, 5th ed. Philadelphia: Churchill Livingstone, An Imprint of Elsevier, 2008.
Acknowledgements
Written by: Teresa Liang
Edited by: Anne Marie Jekyll, MD (Pediatric Resident)
Images
(Image from Rijn R, McHugh K. Rickets Imaging. eMedicine (Last Updated March 18, 2009). Available from http://emedicine.medscape.com/article/412862-print [Accessed on March 5, 2011])
(Image from Rijn R, McHugh K. Rickets Imaging. eMedicine (Last Updated March 18, 2009). Available from http://emedicine.medscape.com/article/412862-print [Accessed on March 5, 2011])
(Image from Rijn R, McHugh K. Rickets Imaging. eMedicine (Last Updated March 18, 2009). Available from http://emedicine.medscape.com/article/412862-print [Accessed on March 5, 2011])
(Adapted from Adam A, Dixon A. Adam: Grainger & Allison’s Diagnostic Radiology, 5th ed. Philadelphia: Churchill Livingstone, An Imprint of Elsevier, 2008)
(Adapted from Adam A, Dixon A. Adam: Grainger & Allison’s Diagnostic Radiology, 5th ed. Philadelphia: Churchill Livingstone, An Imprint of Elsevier, 2008)
(Image from Kirpalani A, Babyn P. Imaging in Osteogenesis Imperfecta. eMedicine (Last Updated August 5,2009). Available from http://emedicine.medscape.com/article/411919-print [Accessed on March 5, 2011])







 (18 votes, average: 3.89 out of 5)
(18 votes, average: 3.89 out of 5)