Click for pdf: Meningitis
Background
General Presentation
Meningitis is an important infectious disease to rule out in the pediatric population because it can have serious medical and social complications. Sequelae include deafness, seizures, learning difficulties, and blindness. Morbidity and mortality rates are high, especially in the neonatal period. Approximately 25-30% of septic neonates have meningitis.
The most common signs and symptoms of meningitis in the neonate population are poor feeding, nausea, vomiting, irritability, and lethargy, which are non-specific constitutional symptoms. The majority (>80%) of patients have fever. Many present with a recent history of URTI, some with apnea, cyanosis, and respiratory distress.
Bacterial meningitis in the older child is usually characterized by hedache, and/or a change in the level of mental status. In severe cases, patients can present with coma. 20-30% of patients experience focal neurological deficits during the first three days of herpes simplex virus (HSV) encephalitis. HSV encephalitis may also cause temporal lobe seizures. Cranial nerve dysfunctions may manifest as symptoms of deafness / vestibular dysfunction (CN XIII), extraocular muscle paralysis (CN III, IV, VI), or facial nerve paralysis (CN VII). Finally, in 30-60% of patients an inappropriate secretion of ADH may occur (SIADH), resulting in hyponatremia and fluid overload.
Physical findings include a change in mental status, bulging anterior fontanelles in the case of the neonate, photophobia and phonophobia, nuchal rigidity, Kernigs and Brudzinski signs, a petechial rash (most often with N. meningitides infection), evidence of dehydration secondary to vomiting, and evidence of increased intracranial pressure such as hypertension, papilledema, and 6th nerve palsy.
Definitions
- Meningitis – Inflammation of the meninges lining the dura, arachnoid space, or pia mater. It can broadly be divided into bacterial meningitis and aseptic meningitis.
- Bacterial Meningitis – Meningitis caused by bacteria (See table 2 in the Appendix for different types). Bacterial meningitis has been declining since the routine use of the H. influenzae type B and S. Pneumonia vaccines. The infecting bacteria often reach the subarchnoid space via hematogenous spread. The resulting inflammatory response causes edema of the surrounding tissue which contributes to the compromise of cerebral perfusion. This may result in ischemia, cerebral edema and an increase in intra-cranial pressure and uncal herniation.
- Aseptic meningitis: An inflammation of the meninges caused by non-bacterial organisms, chemical agents, or other disease processes. Per definition, there is presence of CSF inflammation (pleocytosis and increased proteins) but there is no evidence of bacterial infection on Gram stain. Most cases (80%) of aseptic meningitis are caused by enteroviruses (e.g. coxsackievirus, enterovirus, echovirus, and poliovirus (rare)). Other causes include HSV Types 1 and 2, HIV, Varicella-Zoster, parasites, fungi, systemic diseases (e.g. leukemia, lupus), and IVIg therapy.
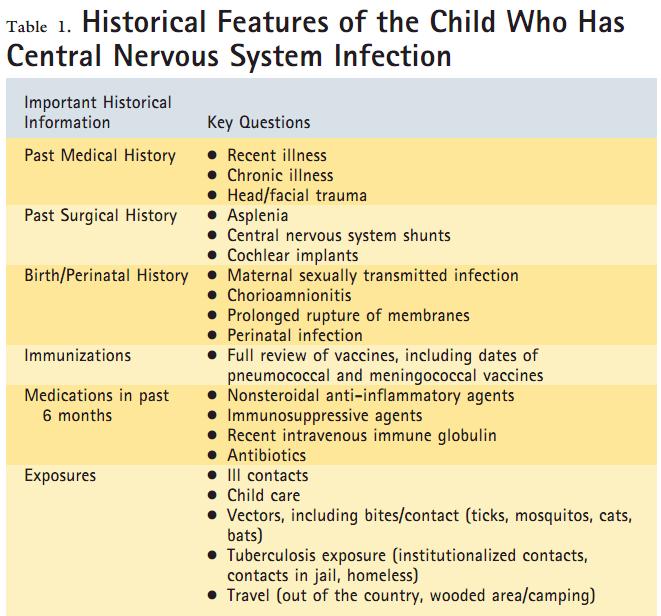
Questions to Ask
– Recent infections: URTI such as otitis media, sinusitis, mastoiditis
– Risk factors predisposing a child to meningitis: 20-25% of children with meningitis have predisposing risk factors. Medical risk factors include immunodeficiency (HIV infection, asplenia, chronic renal disease, sickle cell disease). Mechanical risk factors include CNS trauma, cochlear implants, ventricular shunt placement, and CSF leak.
– Birth history: especially in infants, maternal GBS colonization status and treatment and maternal history of STI should be elicited.
– Contact with ill individuals and travel history
– Medications and immunization status
Physical examination
General inspections include patient’s general appearance, vital signs, a systemic exam and a full neurological examination.
1. Assess the child’s general appearance. Note whether he/she looks sick or not sick. The septic child that also has bacterial meningitis may be either very irritable or lethargic.
2. Note the Vital signs, including temperature. The respiratory rate may be elevated if there is respiratory distress secondary to SIADH and fluid overload, or depressed in cases of hypoventilation secondary to an increase in ICP or encephalopathy. Hypotension and tachycardia may be present if the patient is also septic.
3. On the systemic examination look for a purpuric rash associated with Meningococcemia. Assess for signs of acute otitis media, mastitis, sinusitis or orbital cellulites, infections which could spread to the meninges by direct extension. Also look for other sources of infection such as pneumonia which can spread by hematologic spread. Assess for hydration status and signs of fluid overload on the cardio-respiratory examination. Bradycardia, hypotension and irregular respirations (Cushing’s Triad) could signal increased ICP secondary to cerebral edema or an intracranial abscess.
4. A full neurological exam should be done to rule out any focal neurological deficits. Especially note level of consciousness, signs of increased ICP (the presence of papilledema, diplopia, unilateral or bilateral dilated, poorly reactive pupils, bulging frontanelles in infants).
In a child, signs of meningial irritation/meningismus should be elicited – nuchal rigidity, Kernig sign (patient lies supine with thigh flexed at right angle to trunk, it is positive if knee extension elicits pain in the neck) and Brudzinski signs (patient lies supine with neck flexed, it is positive if patient also reflexively flexes lower extremities)
In young infants, paradoxic irritability is the usual sign of meningeal irritation – the infant prefers to remain motionless and becomes markedly irritable when handeled.
Laboratory Investigations
- Lumbar puncture
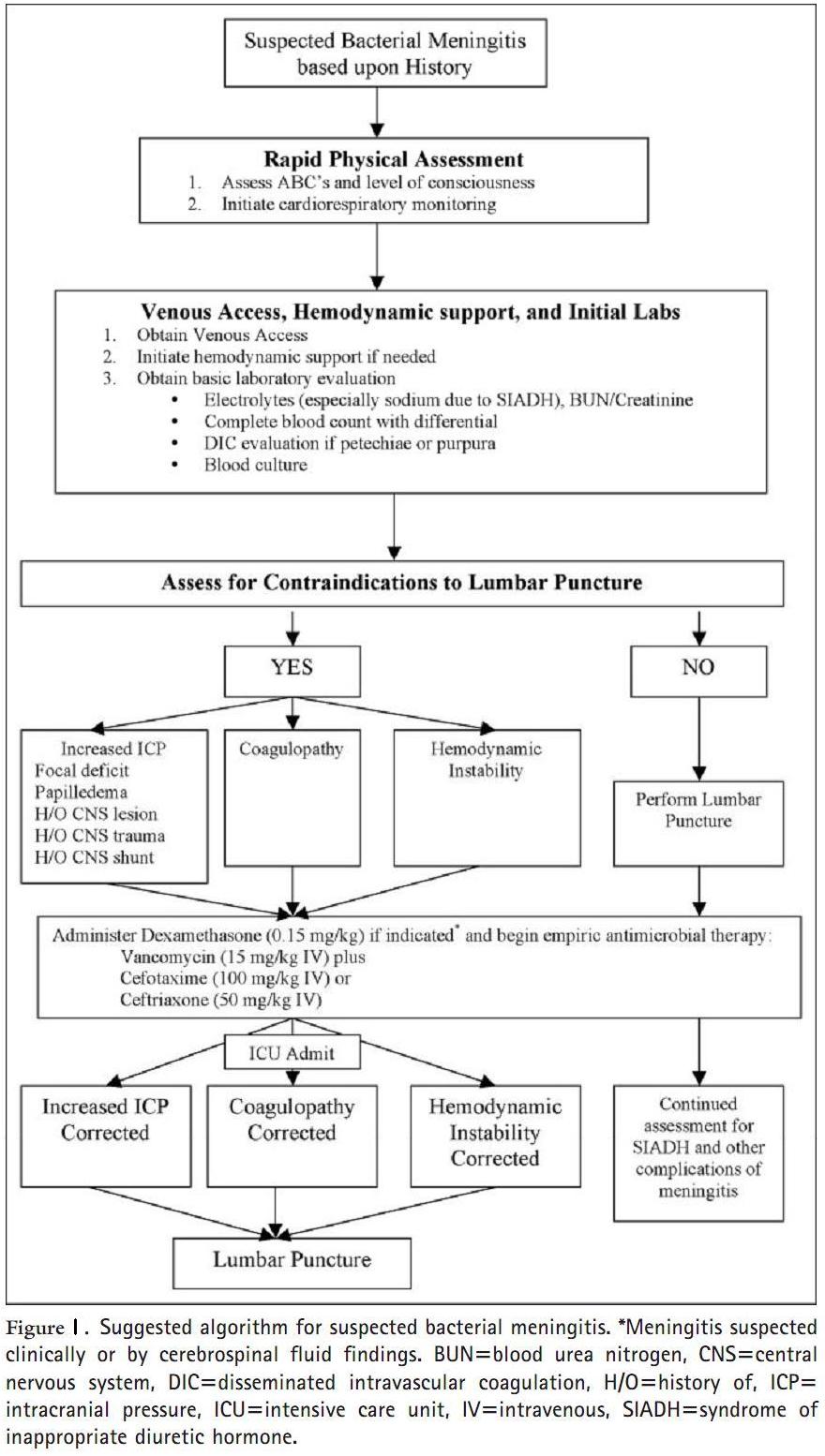
- A lumbar puncture needs to be performed to rule out meningitis. It is especially important to perform a lumbar puncture and examine the CSF in neonates and infants who are febrile without an obvious source of infection. Before performing a lumbar puncture it is important to rule out increased cranial pressure caused by a space-occupying lesion (abscess). A CT scan of the head should be obtained prior to performing a lumbar puncture if there is any concern of increased ICP.
- Cerebrospinal Fluid Findings
- Be sure to send samples for:
- Hematology – cell count and differential
- Chemistry – lactate, glucose (compared with serum glucose taken within 30 minutes of the LP), and protein.
- Microbiology – Gram stain and bacterial culture
- Virology – includes PCR analysis for HSV, VZV, Enterovirus or other specific viruses in question.
- Be sure to send samples for:
| Opening Pressure (cm H2O) | Leukocytes (per mm3) | Protein(mg/dl) | Glucose(mg/dl) | Glc CSF/Blood ratio | |
| Normal neonate | 8-11 | 0-30 | 20-150 | 30-120 | >50% |
| Normal child | <20 | 0-6 | 20-30 | 40-80 | >50% |
| Bacterial | Elevated( >30) | > 500 | >100 | <40 | <30% |
| Viral | Slightly elevated | < 500 | <100 | >40 | >50% |
| Fungal/Tuberculous | Elevated | < 500 | >100 | <40 | <30% |
Other tests
- complete blood count
- blood cultures
- urine and serum electrolytes (screen for SIADH)
- viral cultures may be obtained through throat swabs and stool samples
- serum polymerase chain reactions to aid in identifying potential viral causes
- antigen detection tests for various body fluids
Treatment
Empiric antibiotic treatment should be started immediately. Preferably, this should be started after the LP has been done. Infants less than one month old should be treated with ampicillin plus gentamicin (or cefotaxime). In children older than 1 month of age vancomycin plus cefotaxime or ceftriaxone should be initiated as empiric therapy.
The CSF usually becomes sterile within 36-48 hours after the initiation of antibiotics. Antibiotics need to be continued for at least 5-21 days after sterilization of CSF depending on the etiology of the meningitis.
Aseptic meningitis is treated supportively and with analgesics. If herpes is suspected then one should also treat with encephalitic doses of Acyclovir.
Dexamethasone has been shown to reduce sequelae of meningitis (e.g. hearing loss) in children affected by H. influenzae meningitis. Its benefit in pneumococcal or meningococcal meningitis is uncertain.
Appendix
| Age | Most Common Bacteria |
| 0 to 1 month |
|
| 1 to 23 months |
|
| 2 to 18 years |
|
Table 2: Bacteria causing bacterial meningitis in different age groups
References
Emedicine: Pediatric Meningitis, bacterial.
Emedicine: Pediatric Meningitis, aseptic.
Migita and Christakis, St. Frances Guide to Pediatrics.
Belfus, Pediatric Secrets, Third Edition
Mann K, Jackson MA. Meningitis. Pediatr Rev. 2008 Dec;29(12):417-29; quiz 430. PubMed PMID: 19047432.
Acknowledgements
Writer: Tommy Gerschman
Edited by: Elmine Statham, Rui Chen


 (11 votes, average: 4.27 out of 5)
(11 votes, average: 4.27 out of 5)
Only wanna say that this is invaluable , Thanks for taking your time to write this. best vps host | unmetered vps |