Click for pdf: febrile neutropenia
Introduction
The basis of treatment of any malignancy includes aggressive therapies such as radiation or chemotherapy that targets rapidly dividing tumour cells. Because of the lack of specificity, unwanted secondary effects arrest cell division in other cell lines, including those with a rapid turnover such as in the bone marrow. Bone marrow suppression results in leukopenia, especially neutropenia, causing an increased risk of bacterial infection during these periods.
In addition to bone marrow suppression secondary to cytotoxic medications, other causes of neutropenia exist, including viral suppression of the bone marrow, auto-antibodies against neutrophils, inherited syndromes associated with neutropenia, etc. These will not be reviewed here at great length. It is important to note that all children with neutropenia, irrespective of cause be treated as immunosuppressed when presenting with a fever, with or without a source.
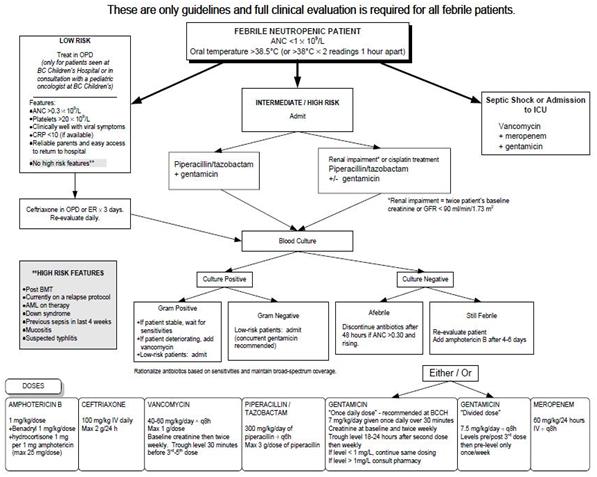
A fever associated with a low neutrophil count is termed febrile neutropenia. As for the particular definitions of “fever” and “neutropenia”, considerable variability exists between sources. The BC Children’s Hospital Fever and Neutropenia Guidelines, put out by the Hematology/Oncology/BMT service, define it as follows:
Neutropenia:
- an absolute neutrophil count (ANC) of <1000/mm3
Fever:
- a single oral temperature of 38.5°C*or
- on oral temperature of 38.0°C measured at two occasions at least an hour apart
* While rectal measurement most accurately reflects core body temperature, there is a risk of bacterial translocation during the process of thermometer insertion into the anus; as a result, taking a rectal temperature in this situation is contraindicated.
Management of febrile neutropenia
As per the the BC Children’s Hospital Fever and Neutropenia Guidelines, published by the Hematology/Oncology/BMT service, the recommended initial assessment and management of febrile neutropenic children is as follows:
http://www.childhealthbc.ca/guidelines/category/10-fever-neutropenia
Empiric broad-spectrum antibiotics should be ordered depending on microbiological resistance patterns at a specific facility and individual patient risk factors. Since there are a variety of microorganisms that could cause the infection, drugs that encompass a broad spectrum against both gram-negative and gram-positive bacteria should be considered.
References
- Meckler G and Lindemulder S. Fever and neutropenia in pediatric patients with cancer. Emerg Med Clin N Am 27 (2009): 525-544.
- BC Children’s Hospital Fever and Neutropenia Guidelines. June 2006. http://www.childhealthbc.ca/guidelines/category/10-fever-neutropenia
Acknowledgements
Writer: Michelle Lai
Resident editor- Katryn Paquette


 (4 votes, average: 4.25 out of 5)
(4 votes, average: 4.25 out of 5)