Click for pdf: IUGR-SGA
Definitions:
- Intrauterine growth restriction (IUGR) describes a fetus that has not reached its growth potential because of genetic or environmental factors.
- Small for gestational age (SGA) refers to an infant whose birth weight was below the 10th percentile for the appropriate gestational age.
- Low birth weight (LBW) is defined as a birth weight < 2500g, regardless of gestational age.
- Very low birth weight (VLBW) is a birth weight < 1500g, regardless of gestational age (although these babies are almost always premature).
Note: Although the terms IUGR and SGA are often used interchangeably, they are not synonymous. A newborn may be labelled SGA according to reference population standards if the newborn is constitutionally small but otherwise normal (e.g. born to parents who are small and/or into an ethnic population that is smaller than the reference population). Alternatively, a fetus with delayed growth late in gestation (asymmetric IUGR) may not have a reduction in birth weight significant enough to be classified as SGA.
Pathophysiology:
The causes of IUGR can be divided into fetal, placental, or maternal factors. More than one factor may be involved, and in many cases a specific etiology cannot be identified.
| Fetal factors | Placental factors | Maternal factors |
| Chromosomal disordersCongenital anomaliesMultiple gestationInfection (e.g. TORCH*, malaria, varicella)
Metabolic disorders |
Uteroplacental insufficiencyAbnormal implantationVascular anomaliesPlacental abruption
Infarction Tumour Villous placentitis (bacterial, viral, parasitic) Confined placental mosaicism |
Chronic illness (e.g. diabetes**, hypertension, renal disease, anemia, pulmonary disease)Pre-eclampsiaEarly or advanced ageMalnutrition
Uterine malformations Substance abuse (e.g. cigarettes, alcohol, narcotics, cocaine) Medications (e.g. warfarin, anticonvulsants) |
*TORCH: Toxoplasmosis, Other (syphilis), Rubella, Cytomegalovirus, Herpes simplex virus
**While diabetes can cause restricted fetal growth, it typically causes excessive growth resulting in a fetus who is large for gestation age (LGA).
Approach to IUGR:
Accurate dating of the pregnancy is essential! Dating is estimated based on the last menstrual period using Nägele’s rule (estimated due date = LMP – 3 months + 7 days). If the dating of the pregnancy is in question, the gestational age can also be assessed by first trimester ultrasound measurement of the crown-rump length. If these estimates differ by more than 7 days, ongoing ultrasound measurements are done every 2-4 weeks to assist with dating and estimating fetal growth.
In general, screening for IUGR relies on symphysis-fundal height measurements as part of routine prenatal care. Ultrasound is used to confirm IUGR based on estimated fetal weight and measurements of head & abdominal circumference.
Once IUGR has been identified, you can use the growth pattern can help to establish the cause. There are two main growth patterns seen in IUGR: symmetric and asymmetric.
| Symmetric | Asymmetric |
| 20-30% of IUGR | 70-80% of IUGR |
| Usually occurs early in pregnancy | Usually occurs later in pregnancy (3rd trimester) |
| Head circumference, length, and weight are decreased proportionally | Head circumference is spared relative to decreased weight, length, and/or abdominal circumference |
| Thought to result from an intrinsic (i.e. genetic) or first-trimester insult (e.g. infection) that interferes with early fetal cellular hyperplasia, producing uniformly reduced growth | Thought to result from adaptation to a hostile environment by redistributing blood flow in favour of vital organs (e.g. brain, heart) at the expense of nonvital fetal organs (e.g. liver, kidneys) |
Investigations:
After identifying a fetus with IUGR, an accurate and thorough history and physical examination are the most important tools for differentiating fetal from maternal and placental causes.
The following investigations are used to direct antepartum management and optimize fetal outcomes:
- Serial measurements of blood flow velocity in fetal vessels using Doppler ultrasound
- Absent or reversed end diastolic flow in the umbilical artery suggests the fetus is in poor condition)
- Non-stress test
- Biophysical profile (a composite score based on fetal breathing movements, gross body movements, fetal tone, fetal heart rate, and qualitative amniotic fluid volume)
- Serial fetal weight assessments
- Amniotic fluid volume
- A detailed fetal anatomic survey by ultrasound (as major congenital anomalies are frequently associated with fetal growth restriction): Omphalocele, congenital diaphragmatic hernia, skeletal dysplasia and congenital heart defects are among the congenital anomalies associated with failure to maintain normal fetal growth
Other studies, such as testing for congenital infections or karyotype (chromosomal analysis), are considered on an individual basis depending on risk factors and other clinical features. A course of antepartum steroids is recommended for preterm fetuses to promote lung maturation.
Timing of Delivery:
The timing of delivery in a preterm growth restricted fetus should be guided by both fetal condition and gestational age. The fetus should be delivered if the risk of fetal death exceeds the risk of neonatal death. When IUGR is mild and uncomplicated, with normal end-diastolic flow, delivery can be delayed until 37 weeks to allow time for lung maturation.
Complications:
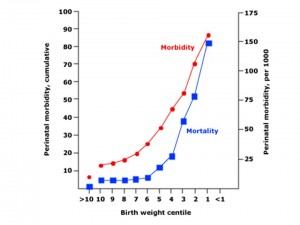
Infants with IUGR have greater morbidity and mortality than do appropriately grown, gestational age–matched infants. Neonatal complications include:
- Hypoglycemia
- Hypothermia
- Polycythemia
- Asphyxia
- Jaundice
Therefore, when you are caring for an infant with IUGR/SGA, you must anticipate – and wherever possible, prevent – the above complications.
At birth, initial measures are the same as for infants of normal weight. Additional considerations include the need to maintain body temperature (ideally between 36.5-37°C), monitoring of the heart rate and respiration, serum glucose screening, and special attention to the details of feeding. Meticulous infection control is also required, as these infants have an increased susceptibility to infection.
If the infant is also premature, there are many other complications one must look out for including potential respiratory, cardiovascular, hematologic, gastrointestinal, renal, metabolic, and central nervous system problems.
Figure 1: SGA Morbidity and Mortality. Adapted from Up To Date, 2009.
Infants with symmetric SGA, including those who are constitutionally small, are most likely to have permanent growth restriction. In the absence of congenital abnormalities or central nervous system injury, those with asymmetric growth restriction are more likely to experience catch-up growth under optimal childhood conditions (usually by the second year of life).
IUGR infants are at greater risk of neurobehavioural disorders including impaired school performance, social skills, and fine motor control.
As adults, IUGR infants are at risk for significant metabolic conditions (obesity, type 2 diabetes mellitus) and cardiovascular disorders (ischemic heart disease, hypertension). The fetal origins hypothesis of adult morbidities may be due to insulin resistance, which may be evident in early childhood.
Recurrence Risk:
In successive pregnancies, there is a tendency to repeat IUGR/SGA deliveries. To reduce this risk, any potentially treatable causes should be addressed. (e.g. smoking cessation, appropriate nutrition).
Summary:
Intrauterine growth restriction occurs when a fetus fails to meet its growth potential as a result of intrinsic or environmental factors; it may be symmetric or asymmetric. Small for gestational babies are infants whose birthweight falls less than the 10th percentile. Fetal growth restriction requires thorough evaluation and management during the antepartum, intrapartum and postpartum periods. These infants are at higher risk for neonatal complications that must be monitored closely as well as long term pediatric follow up for potential long term complications.
References:
Kleigman RM, Marcdante KJ, Jensen HB, Behrman RE. Nelson Essentials of Pediatrics 5th Edition. Elsevier Saunders 2006.
Oelberg, DG. Prenatal Growth: The Sum of Maternal, Placental, and Fetal Contributions. Pediatrics in Review 2006; 27: 224 – 229.
Russell, BK. Babies Who Are Small for Gestational Age. Pediatrics in Review 1995; 16:9, 354.
Resnik, R. Fetal growth restriction: evaluation and management. Up to Date 2009. www.uptodate.com
Divon M, Ferber A. Overview of the causes and risk factors for fetal growth restriction. Up to Date. www.uptodate.com.
Acknowledgements:
Written by: Jennifer Smitten
Edited by: Anne Marie Jekyll


 (40 votes, average: 4.23 out of 5)
(40 votes, average: 4.23 out of 5)