Click for pdf: Pediatric Fractures
Introduction
The anatomy and biomechanics of pediatric bone differ from that of adult bone, leading to unique pediatric fracture patterns, healing mechanisms, and management. In comparison to adult bone, pediatric bone is significantly less dense, more porous and penetrated throughout by capillary channels. Pediatric bone has a lower modulus of elasticity, lower bending strength, and lower mineral content. The low bending strength induces more strain in pediatric bone than for the same stress on adult bone and the low modulus of elasticity allows for greater energy absorption before failure. The increased porosity of pediatric bone prevents propagation of fractures, thereby decreasing the incidence of comminuted fractures. The pediatric periosteum is extremely strong and thick, functioning in reduction and maintenance of fracture alignment and healing.
Anatomy of pediatric bone
Pediatric long bones have three main regions: epiphysis, physis and metaphysis.
Epiphysis: each end of a long bone with associated joint cartilage.
Physis (growth plate): cartilage cells that create solid bone with growth.
Metaphysis: wide area below the physis, closest to the diaphysis/shaft.
Another key component of bone is the periosteum, which is a thick, nutrient layer that wraps circumferentially around bones. It serves a major role in healing the outer layer of bone.
Pediatric fracture patterns
The mechanisms of fracture change as children age. Younger children are more likely to sustain a fracture while playing and falling on an outstretched arm. Older children tend to injure themselves while playing sports, riding bicycles, and in motor vehicle accidents. Also, because a child’s ligaments are stronger than those of an adult, forces which would tend to cause a sprain in an older individual will be transmitted to the bone and cause a fracture in a child. Caution should therefore be exercised when assessing a young child diagnosed with a sprain.
Plastic Deformation
- A force produces microscopic failure on the tensile/convex side of bone which does not propagate to the concave side. The bone is angulated beyond its elastic limit, but the energy is insufficient to produce a fracture.
- No fracture line is visible radiographically.
- Unique to children
- Most commonly seen in the ulna, occasionally in the fibula.
- Bend in the ulna of < 20° in a 4 year old child should correct with growth.
Buckle fracture
- Compression failure of bone that usually occurs at the junction of the metaphysis and the diaphysis
- Commonly seen in distal radius.
- Inherently stable
- Heal in 3-4 weeks with simple immobilization.
Greenstick fracture
- Bone is bent and the tensile/convex side of the bone fails.
- Fracture line does not propagate to the concave side of the bone, therefore showing evidence of plastic deformation.
- If the bone undergoes plastic deformation, it is necessary to break the bone on the concave side to restore normal alignment, as the plastic deformation recoils the bone back to the deformed position.
Complete fracture
- Fracture completely propagates through the bone.
- Classified as spiral, transverse, or oblique, depending on the direction of the fracture line.
- Spiral fractures:
- Created by a rotational force.
- Low-velocity injuries
- An intact periosteal hinge enables the orthopedic surgeon to reduce the fracture by reversing the rotational injury.
- Oblique fractures:
- Occur diagonally across the diaphyseal bone at 30° to the axis of the bone.
- Unstable, therefore alignment is necessary.
- Fracture reduction is attempted by immobilizing the extremity while applying traction.
- Transverse fractures:
- Created by a 3-point bending force.
- Easily reduced by using the intact periosteum from the concave side of the fracture force.
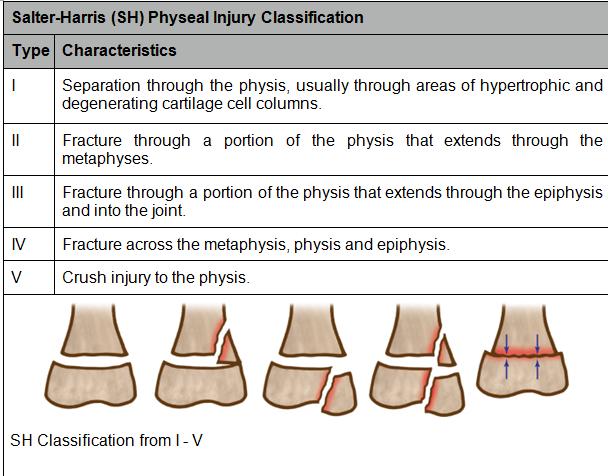
Physeal fractures
- Fractures to the growth plate can be caused by i) crushing, ii) vascular compromise of the physis or iii) bone growth bridging from the metaphysis to the bony portion of the epiphysis.
- Damage to growth plate may result in progressive angular deformity, limb-length discrepancy or joint incongruity.
- The distal radial physis is the most frequently injured physis.
- Most physeal injuries heal within 3 weeks. This rapid healing provides a limited window for reduction of deformity.
- Physeal injuries are classified by the Salter-Harris (SH) classification system, based on the radiographic appearance of the fracture.
Image Source: Kliegman RM et Al. Nelson Essentials of Pediatrics. Saunders; 2007, p 2838
Differences between pediatric and adult fracture healing
Fracture Remodeling
- Process that occurs over time as a child’s bone reshapes itself to an anatomic position.
- The amount of remaining bone growth provides the basis for remodeling. Thus, the younger the child, the greater remodeling potential, and the less important reduction accuracy is.
- Occurs over several months following injury.
- Factors affecting amount of remodeling:
- Age: younger children have greater remodeling potential.
- Location: fractures adjacent to a physis undergo greatest amount of remodeling.
- Degree of deformity
- Plane of deformity with respect to adjacent joint: remodeling occurs more readily in the plane of a joint than with deformity not in the plane of the joint.
Overgrowth
- Caused by physeal stimulation from the hyperemia associated with fracture healing.
- Prominent in long bones (ex. femur).
- Growth acceleration is usually present for 6 months to 1 year following injury.
- Does not present a continued progressive overgrowth unless complicated by a rare arteriovenous malformation.
- > 10 years of age, overgrowth is less of a problem and anatomic alignment is recommended.
Progressive Deformity
- Injuries to the physis can be complicated by progressive deformities with growth.
- The most common cause is complete or partial closure of growth plates.
- Deformities can include angular deformity, shortening of bone, or both.
- The magnitude of deformity depends on the physis involved and the amount of growth remaining.
Rapid Healing
- Pediatric fractures heal more quickly than adult fractures due to children’s growth potential and a thicker, more active periosteum (the periosteum contributes the largest part of new bone formation around a fracture)
- As children reach their growth potential, in adolescence and early adulthood, the rate of healing slows to that of an adult.
- There is one downside to rapid healing, however; refractures.
Assessment
As with most problems in medicine, the initial approach to fractures includes a thorough history and physical exam.
Practitioners must keep in mind that a young child may not be able to describe bony pain or the circumstances of injury. Hence, toddlers and non-verbal children may simply present with the refusal to weight bear or move the injured area, irritability, or due to a caregiver’s observation of a new deformity.
Questions to include in the history of a child presenting with a suspected fracture include:
Characterization of the Pain and Presenting Symptom:
- Location: is the pain localized to a particular region or does it involve a larger area?
- Intensity: use a pain scale from 1-10.
- Quality of pain
- Onset of pain
- Duration of pain
- Progress of pain: is it static, increasing or decreasing?
- Is the pain radiating?
- Any aggravating or alleviating factors?
Other considerations:
- Indicators of compromised neurovascular status (e.g.: change in or loss of sensation, cold, pale, paralyzed limb)
- Mechanism of injury
- Possibility of non-accidental injury or child abuse, particularly in a child with limited physical mobility, with an injury out of proportion to the mechanism, with multiple injuries, or with a suspicious mechanism of injury (e.g.: a 2 month old baby who developmentally cannot roll, but who “rolled off the changing table”)
- Rare possibility of underlying bone abnormality (family history of fractures, bone or collagen disorders, prior fractures, mechanism out of proportion to injury).
Physical examination should include assessment of the joint in question and, whenever non-accidental injury may be a possibility, a screening exam of the entire skeleton, fundoscopy, as well as an abdominal and cutaneous appraisal for other signs of trauma. One should always examine a joint above and below the symptomatic one. Important features to include in the examination of all fractures are:
Inspection
- Patient movement
- Discrepancy in limb length
Palpation
- Assessment of local temperature, warmth, tenderness
- Existence of swelling or mass
- Tightness, spasticity, contracture
- Bone or joint deformity
- Evaluate anatomic axis of limb
Range of Motion
- Assess and record the active and passive range of motion of the joint
Neurovascular assessment of the injured area
- Inspect the color of the limb
- Palpate for pulses, and to elicit appropriate sensation to touch, temperature
- If possible, elicit strength in neighboring muscle groups
Finally, plain radiographs are the first step in evaluating most musculoskeletal disorders. When indicated, advanced imaging may include nuclear bone sans, ultrasonography, CT, MRI and PET scans.
Differential diagnosis
Common Causes of Adult Fractures
| Cause | Pathology | Presentation | Investigation |
| Osteoporosis | – Post-menopausal women- Calcium deficiency and estrogen deficiency → decreased bone mineral density | – Fractures of axial skeleton, typically mid-thoracic vertebra, hip | – Dual X-ray absorptiometry scan of the spine, hip or forearm to measure bone mineral density |
| Osteomalacia | – Lack of vitamin D and metabolite disturbances → defective mineralization of bone matrix | – Fractures of the pelvis and long bones | – Measure 25-hydroxyvitamin D levels |
| Osteitis deformans (Paget’s disease) | – Unknown cause- Localized metabolic bone condition → breakdown → abnormal, weak bone formation → pain and deformity | – Fractures after trauma, typically in femur, tibia and forearm- Bowing of long bones | – Bone X ray- Raised serum alkaline phosphatase |
| Multiple myeloma | – Neoplasms of mature and immature plasma cells → typically involves skeleton → bone destruction | – Pathologic fractures | – Bone marrow biopsy |
Common Causes of Pediatric Fractures
| Cause | Pathology | Presentation | Investigation |
| Child abuse | – 30-50% of children seen by orthopedic surgeons are the victims of non-accidental injury | – Femur- Distal femoral metaphyseal corner- Posterior rib- Scapular spinous process- Proximal humeral | – Diagnosis requires multiple factors: history, clinical presentation, behavioural and physical observation. |
| Birth Injury | – Potential complication of forceps delivery- Complication of cephalo-pelvic disproportion and shoulder dystocias | – Clavicular fractures- Humeral fractures- Femoral fractures | – X Ray- Cephalohematoma at the site of injury and calcification around fracture will help indicate if fracture occurred during birth or after. |
| Rickets | – Lack of vitamin D and metabolite disturbances → defective mineralization of bone matrix- Similar to osteomalacia in adulthood | – No specific fracture pattern- May present with bowed limbs, “rickety rosary”, craniotabes | – Measure 25-hydroxyvitamin D levels |
| Osteomyelitis | – Acute or chronic infection of bone → lesions of the metaphyses | – Long bones | – Upon suspicion, immediate referral to orthopedic surgeon for body fluid tests, aspiration of bone and imaging |
| Copper deficiency | – Copper deficiency → impaired bone calcification | – No specific fracture pattern | – Slit-lamp examination for Kayser-Fleischer rings- Serum ceruloplasmin and 24-h urinary copper excretion- Liver biopsy |
Management
Although primary prevention of fractures is ideal, fractures remain a common presentation in pediatrics. Due to their immature, growing bones, care providers must remain vigilant regarding potential fractures, as they may present with subtle signs and symptoms. A high index of suspicion and appropriate treatment of orthopedic injuries can prevent the long-term morbidity associated with stunted growth potential and deformed limbs.
References
- Calmar, A., Vinci, RJ. The anatomy and physiology of bone fracture and healing. Clinical Pediatric Emergency Medicine 2002; 3(2):86-93.
- Jenny C, Evaluating infants and young children with multiple fractures. Pediatr Rev 2006; 118(3):1299-1303.
- Behrman RE, Kliegman RM, Arvin AR, eds. Chapter: Common Fractures. Nelson’s Textbook of Pediatrics. 16th ed. Philadelphia, Pa: WB Saunders Co; 2007: 2834-2841
- Neil E. Green, Marc F. Swiontokowski. Skeletal Trauma in Children. Saunders, Philadelphia. 1992.
- Staheli LT. Fundamentals of Pediatric Orthopedics. 3rd ed. Philadelphia, Pa: Lippincott-Raven Publishers; 2003
- The Merck Manuals. Nutritional Disorders: Copper [Internet]. 2008 [updated 2008, cited 2011 Jan 16]. Available from: http://www.merckmanuals.com/professional/sec01/ch005/ch005c.html
Acknowledgements
Author: Laura Budd
Editor: Katryn Paquette, MD.,CM. (Pediatrics Resident)


 (27 votes, average: 4.30 out of 5)
(27 votes, average: 4.30 out of 5)