Click for pdf: Lumbar_puncture_in_pediatrics
Background
Although the attempts at retrieval and analysis of the cerebrospinal fluid date back well over a century, it was not until the 1950s when the lumbar puncture was widely popularized. Then workup of any significant central nervous system condition was not considered complete until a lumbar puncture was performed. Since then, the advent of modern medical imaging has contributed to steering away from this trend, fortunately leading to a decrease in unnecessary administration of this invasive procedure and associated complications. Lumbar puncture, however, still plays a critical role in both pediatric medical diagnosis and treatment today.
This brief overview will primarily focus on the procedure and its diagnostic utility.
Basic Anatomy and Physiology
The Cerebrospinal Fluid
The adult human brain and spinal cord literally float in approximately 150cc of cerebrospinal fluid (CSF). About 500cc of CSF is produced by choroid plexus each day. These volumes, naturally, are significantly lower for a neonate and increase with age until adulthood. The CSF is mainly produced by the choroid plexus within the lateral ventricles. CSF is essentially a blood ultra-filtrate and therefore its composition resembles that of plasma. Among the differing parameters, its glucose content is lower than that in blood and the normal range of CSF/blood ratio varies with age. Although the osmolality of the two fluids is equal, the protein content of CSF is markedly less relative to plasma.
Once CSF leaves the lateral ventricles, it flows through the foramina of Monroe into the midline third ventricle. Next, the CSF passess through the aqueduct into the fourth ventricle where it flows through the foramen of Magendie (midline) and foraminae of Luschka (lateral) into the cisterna magna. The cisterna magna is continuous with the subarachnoid space surrounding both the brain and the spinal cord. The CSF is then reabsorbed back into the venous circulation via arachnoid villi.
Diagnostic use of CSF analysis
Analysis of the cerebrospinal fluid can yield an important insight into the underlying pathological processes CSF can be analyzed for the presence of RBCs and WBCs (with differential), bacteria (Gram stain and other stains, culture and sensitivity), viruses (culture, PCR), as well as glucose and protein levels. Other more sophisticated tests, such as neurotransmitter levels and metabolic markers may also be performed in certain scenarios.
The procedure: surface landmarks
It is critical that you first orient yourself with respect to the lower back landmarks before attempting the puncture. An ideal patient for this procedure is one that is lean and whose boney prominences are readily visible. In the real world, however, seemingly simple localization of anatomic landmarks may sometimes turn out to be a challenge. Once the patient is properly positioned (read on for positioning instructions), you should identify the spinous processes of the spinal column by palpating them. Make sure no anomalies are present. Palpate the cephalad aspects of the iliac bones, the iliac crests laterally. The line connecting the iliac crests should correspond to approximately the L4 spinous process, one to two interspaces above the optimal space to access the subarachnoid space.
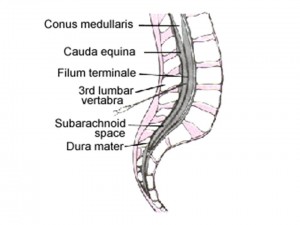
Relevant deep anatomy
The spinal cord typically terminates at the level of L1 vertebral body in an adult and slightly lower in a child. Below that level there are only spinal nerve roots traveling within the lumbar cistern to reach their respective intervertebral foramina from where they exit the dural sack. Because of their resemblance of a horse’s tail, this nerve bundle is referred to as cauda equina. The distal tip of the spinal cord gives rise to filum terminale, a fibrous structure that travels among the spinal nerve roots to finally attach to the dorsum of the coccyx, anchoring the spinal cord and the dural sac distally.
From a point of view of a spinal needle, the structures that are penetrated, from superficial to deep, are as follows (this is a favourite anesthesia rotation question!):
- skin
- subcutaneous connective tissue
- supraspinous ligament
- interspinous ligament
- ligamentum flavum
- epidural space
- dura mater (dural sac)
- subarachnoid space (lumbar cistern with CSF)
Indications, contra-indications and complications
Whenever performing an invasive procedure on a patient, you must always weigh the potential benefit to the potential risks. Undoubtedly, diagnosis of such serious conditions as meningitis or subarachnoid hemorrhage carries benefits for an ill patient, if appropriate course of treatment is undertaken. Below there is listed clinical indications as well as contraindications. Keep in mind, however, that there is a continuous evolving debate in pediatric literature around these.
To obtain informed consent, make sure to inform the patient or guardian of potential complications reviewed below.
Indications
- Suspected meningitis or encephalitis
- Suspected subarachnoid hemorrhage, only if CT scan is normal
- Diagnosing or ruling out sepsis in the neonatal period
- Other indications include diagnostic workup of certain malignancies, seizures, metabolic disorders and other neurological conditions (e.g. MS, GBS)
Contraindications
- Coma
- Suspected raised intracranial pressure
- Cardiovascular compromise
- Respiratory compromise
- Suspected cerebral herniation
- Coagulopathy/thrombocytopenia
- Local infection at lumbar puncture site
- Vertebral anomalies
Complications
- Postdural puncture headache (relatively common)
- Local back pain
- Infection
- Spinal hematoma
- Subarachnoid epidermal cyst
- Apnea
- Transient limp or pararesthesias
- Transient ocular palsy
- Cerebral herniation
Equipment
Usually a prepackaged commercial kit containing:
- 20 gauge spinal needle (different kinds are available, e.g. Quincke)
- syringes and needles (22 and 25 gauge) for spinal anesthesia
- manometer with stopcock
- sterile drapes, gauzes, brushes and bandages for prepping skin
- local anesthetic
Technique
Especially pertinent to pediatrics, a topical anesthetic (e.g. EMLA cream) can be applied 30 to 60 minutes before performing the puncture to minimize pain on penetration.
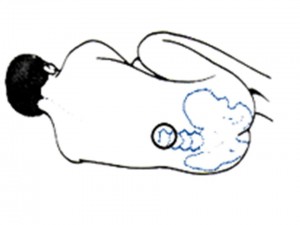
Either a sitting or lateral decubitus position can be used for lumbar puncture. Whichever approach is chosen it is important to monitor the patient visually and with pulse oximetry for any signs of respiratory difficulty as a result of assumed position. Have somebody help you hold the patient still to ensure adequate restraint during the procedure.
The subarachnoid space must be entered below the level of spinal cord termination. Any of the interspaces between L3-L4 and L5-S1 can be used for the lumbar puncture in kids. Whether the lateral decubitus or sitting position is chosen, the spine should be flexed maximally to increase spacing between spinous processes. Extensive neck flexion, however, should be avoided to minimize a chance of respiratory compromise. Make sure the hips and shoulders are aligned and that the back is perpendicular to the bed surface.
The procedure should be performed using sterile technique. The patient’s back should be carefully prepared and draped using provided disinfecting solution and drapes. Orient yourself anatomically and find the L4 spinous process at the level of iliac crests (as described above). Palpate a suitable interspace distal to this level. Infiltrate 2% Lidocaine subcutaneously (without epinephrine to prevent cord infarction should it be introduced into the cord by accident) with a fine needle. A field block can be applied injecting into and on either side of the interspinous ligaments. This anesthetizes not just the skin, but also the interspinous ligaments, muscles, and the periosteum.
Once the patient is properly positioned, the area sterilized and draped and adequate anesthesia of the area achieved, the spinal needle can be introduced. Identify the two spinal processes in between which the needle will be introduced, penetrate the skin and slowly advance the tip of the needle at about 10 degrees cephalad (i.e. toward the patient’s umbilicus). Following penetration of skin, resistance will be encountered as the tip of the needle passes through interspinous ligaments. Remember to frequently stop advancing the needle and check for the presence of CSF by removing the stylet. You may feel a characteristic “pop” indicating entrance into the subarachnoid space. If the needle is no longer progressing and resistance encountered, it is likely that you have hit bone. Withdraw the needle leaving the tip in, recheck the landmarks and slowly progress the needle again.
You should attempt to measure the opening pressure using the manometer by attaching it via a stopcock to the spinal needle. Normal opening pressure is 7 to 15 cm H2O. Always make sure to hold the spinal needle securely between your thumb and index finger and brace your hand against the patient’s back, especially when putting in or removing anything from it.
Collecting a Sample
To collect a CSF sample, start with emptying the contents of the manometer into the first collection tube. Once the manometer is empty, detach it and continue with collection straight from the spinal needle. In general, a CSF volume of 1cc obtained in each consecutive tube (usually up to 4 tubes) should be adequate for most analyses. In the neonate, 2ml in total can be safely removed and in an older child 3 to 6 ml can be sampled depending on the child’s size. When collection is finished, replace the stylet and remove the needle from patient’s back. Apply first pressure, then a dressing to the puncture site.
SUPPLEMENTARY INFORMATION
LP VIDEO: http://www.rch.org.au/clinicalguide/forms/lumbarVideo.cfm
Figure 1. Lumbar spine anatomy.
Figure 2. Lumbar puncture: lateral decubitus positioning and surface landmarks.
Figures from: http://www.mtio.com/lupus/prolp.htm
BIBLIOGRAPHY
Fleisher GR and Ludwig S. Textbook of Pediatric Emergency Medicine, 4th ed. Philadelphia: Lippincott Williams & Wilkins, 2000.
Fong B and VanBendegom JM. Lumbar Puncture, Reichman E and Simon RR Emergency Medicine Procedures, 1st ed. McGraw-Hill Professional, 2003.
Guyton AC. Textbook of Medical Physiology, 9th ed. Philadelphia: W B Saunders, 1996.
Reisdorff EJ, Roberts MR, Wiegenstein JG. Pediatric Emergency Medicine. Philadelphia: W B Saunders, 1993.
Waldman AL. Lumbar Puncture (CSF Examination), November 6, 2004, eMedicine.
Acknowledgements
Written by: Blazej Iwo Szczygielski
Edited by: Elmine Statham



 (28 votes, average: 3.93 out of 5)
(28 votes, average: 3.93 out of 5)