In Neurology, there are many indications and situations where pharmacotherapy would be appropriate. The main and probably most common use however, is in seizure management.
A) Overview
- Seizure = paroxysmal involuntary disturbance of brain function in which abnormal neuronal firing is manifested as impairment, loss of consciousness, abnormal motor activity, sensory disturbance, and/or autonomic dysfunction.
- Epilepsy = recurrent spontaneous seizures unrelated to fever or to acute cerebral insult.
- The etiology of seizures are complex and have genetic, molecular, and environmental influences.
- Seizures can present in a variety of forms, and are often classified according to their clinical presentation (ie. partial vs. generalized) (See Appendix for a more detailed list of types of seizures).
- First line treatment for seizures is pharmacotherapy.
B) Pathophysiology
- Initiation of a seizure requires a group of neurons capable of burst discharge and a GABAergic inhibitory system.
- Excitatory neurotransmitters (ie. glutamate) have an effect in producing neuronal excitation by acting on specific cell receptors.
- An epileptic seizure at a basic level represents the imbalance between excitatory and inhibitory neurons.
- Treatment of seizures involves modulating either the excitatory or inhibitory systems.
C) Receptors in the Brain
- There are numerous types of receptors in the brain. Some receptors rely on a second messenger system, while others require complex enzymatic interactions to carry out their physiological functions.
- Other receptors are actually ion channels, or are indirectly linked to an ion channel. These channels are responsible for regulating the movement of ions across the cell membrane thereby maintaining the cell membrane potential and the conduction of electrical signals. Membrane channels also have a variety of other functions; however, for this discussion will focus only on the channels involved in seizures.
- In general, channels can be divided into their effect on the cell’s ability to generate an action potential – that is, whether the activating the channel has an inhibitory or an excitatory effect.
| Excitatory | Inhibitory |
| Na Channels | Chloride Channels |
| Calcium Channels | Potassium Channels |
D) How Channels work:
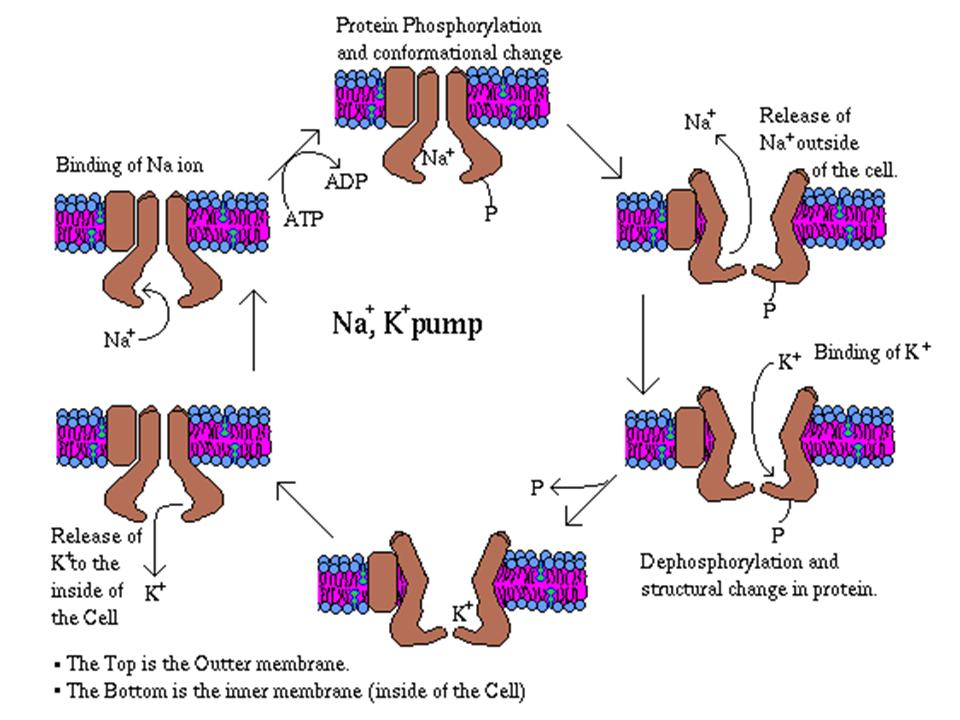
The cell membrane contains an inherent active ability to move certain ions out of the cell, and other ions into the cell.
Therefore, a concentration gradient is established. Because ions are charged, this concentration gradient in turn generates an electrical potential gradient.
- Depending on the direction of the gradient, the movement of an ion may either neutralize (depolarize), or increase (hyperpolarize) the electrical potential. Depolarization conducts a signal along the cell, whereas hyperpolarization does the opposite.
- In general, positive ions moving in depolarize the cell, whereas negative ions moving in will hyperpolarize the cell. The converse is also true in that negative ions moving out depolarize the cell, whereas positive ions moving out will hyperpolarize the cell.
- As a result, Na+ and Ca2+, two of the most common cation channels in the brain, are excitatory.
- Cl-, the most anion channel in the brain, is inhibitory.
- K+ channels, depending on the movement of the ion, can be either excitatory or inhibitory.
- Some channels conduct multiple ions, but are often classified by the ion that flows most readily or has the greatest physiological significance for that channel (ie. some Ca2+ channels conduct Na+ and K+ as well, but Ca2+ is the most readily conducted). Furthermore, channels can be grouped by their activation means – that is, how a channel is controlled or regulated.
- There are two main means for regulation: Ligand gating and Voltage gating
- Ligand gating refers to a channel requiring the binding of a neurotransmitter (NT) or chemical in order to open or to close the channel
-
- The main NTs or ligands of relevance are Glutamate and GABA.
- Glutamate acts on exciatatory cation channels, therefore Glutamate is considered to be an excitatory NT
- GABA acts on inhibitory anion channels (mainly Cl-), therefore GABA is considered to be an inhibitory NT
- Voltage gating refers to a channel requiring a depolarization, or repolarization of the cell membrane in order to open or close the channel. Changes in the membrane potential will alter the conformation of the channel allowing passage of selective charged ions.
- Different channels conducting the same ions may have different gating mechanisms (ie. Voltage gated vs. ligand gated Ca2+ channels)
E) Clinical Correlation:
- Since seizures are uncontrollable bursts of activity between networks of neurons, the traditional approach to treatment has been to disrupt the pathway of communication. Pharmacotherapy accomplishes this goal by interfering with a cell’s ability to signal other cells, or by disturbing the network as a whole.
F) Pharmaco-Physiology:
- Medications can have either an inhibitory effect, or excitatory effect on the generation of the action potential (and in turn, the signaling capability of the cell). Most seizure medications can be generalized as having one or more similar mechanisms:
Inhibiting Na+ channels
- In the brain, the ‘fast depolarization’ is carried by a Na+ current.
- By blocking the Na+ channel itself, an action potential cannot be generated or conducted across the membrane
- There are many types of Na+ channels, including voltage and ligand gated.
- Blocking each specific type of channel produces different physiological effects
- Blocking ligand gated Na+ channels blocks action potential generation at the level of the synapse, and no signal at all is carried through that cell
- Blocking voltage dependant Na+ channels however, blocks action potentials at the level of the axon, or past the synapse. Hence, an initial signal can be generated, but not conducted through the neuron.
- Because Na+ channels are so widely dispersed and crucial to cell function, therapeutic agents must have very specific targets. In the case of seizures, many medications are designed with an inherent ability to bind only to highly active channels (such as those involved in seizure activity) thereby limiting the therapeutic side effects of the medication.
Inhibiting Ca2 channels
- Ca2+ channels have widespread distribution through the CNS, and a large number of functions.
- In the brain, fast and slow depolarization can be carried by Ca2+ channels.
- Different channels can be activated by different ligands, voltage changes, or other stimuli.
- Furthermore, Ca2+ is involved in the regulation of other NT release from the cell synapse.
- Like Na+ channels, inhibiting Ca2+ channels can have a number of different effects, depending on the channel inhibited.
- The many roles and types of channels, however, increases the potential number of physiological effects of inhibition.
- Inhibiting some voltage gated Calcium channels can prevent release of synaptic products, thereby preventing communication across the synapse altogether. Inhibiting other voltage gated channels can prevent the depolarization of neurons involved in cyclic regulation of activity (such as in the thalamus), disrupting cyclic activity in cells (ie. during seizures).
- Inhibiting ligand gated channels, such as those on the post synaptic membrane, can also block signal transmission through a cell, despite the presence of an activating NT
Potentiating K+ channels
- Owing to the differential active movement of ions across the membrane, K+ is in much greater concentration within the cell. Therefore, its movement down its gradient (and out of the cell) leads to a repolarization or hyperpolarization of the cell membrane.
- By modulating K+ currents, some drugs work to hyperpolarize active cells, decreasing their ability to conduct a signal, while others may prevent repolarization of the cell after an action potential, thus also preventing action potential conduction.
Potentiating Cl- Channels
- The movement of anions into a cell increases the polarity of the membrane, thereby increasing the difficulty in generating an action potential.
- Many drugs may actually modify a neurotransmitter associated with a Cl- channel, rather than the channel itself.
Affecting Neurotransmitters
- Some drugs also have a direct effect on neurotransmitters
- Generally, modulation involves inhibition of excitatory NTs (ie Glutamate) or enhancement of inhibitory NTs (ie. GABA).
- Inhibition can occur through a number of mechanisms:
- The NT can be prevented from binding to its target ligand
- The NT can be prevented from being released from the synapse
- The NT can be prevented from being made from its precursors
- The NT and its precursors could be depleted from the presynaptic cell
- or a variety of other mechanisms.
- Potentiation of an inhibitory NT such as GABA can occur through a number of mechanisms as well:
- Increasing the amount or precursor available for production
- Increasing the activity of the enzymes responsible for production
- Inhibiting the NT degradation
- Inhibiting the NT removal
- and other mechanisms.
- Some drugs will also act on the NT targets (either at the same or a different binding site) to modulate the receptor response to a given NT (changing its responsiveness, or changing the outcome response itself).
Common Pediatric and Adult Antiseizure Medications and Mechanisms of Action:
| Drug name | Primary Mechnaism of Action (secondary effects omitted) |
| Benzodiazepines | Potentiate GABA at GABAA channels and increases frequency of channel opening. |
| Carbamazepine (Tegretol) | Binds to sodium channels at high firing frequencies to prolong inactivated state of sodium channel and prevent sustained high frequency action potentials. Also acts presynpatically to inhibit synaptic transmission. |
| Divalproex Sodium (Valproic Acid) | Uncertain? blocks sustained high firing sodium channels; increases GABA concentration through facilitation of Glutamic Acid Decarboxylase. |
| Ethosuxamide (Zarontin) | Inhibits T type Calcium channels in thalamus-> inhibits the rhythm generator function of thalamus and disrupts seizure. |
| Gabapentin | Does not act on GABA receptors; alters GABA metabolism, non synpatic release, and reuptake (leading to increased GABA). |
| Lamotrigine (Lamictal) | Similar to phenytoin – causes selective inactivation of active Na channels leading to suppression of rapid action potentials. |
| Leviteracetam | Main mechanism unknown; allosteric modulation of GABA receptors, High voltage activated Calcium channels, and Potassium channels. |
| Phenobarbital | Unknown; suspected to be enhancement of inhibition and decreased exictation. Stops high frequency action potential firing. |
| Phenytoin, Fosphenytoin(Dilantin) | Alters Na, K, and Ca conductance, membrane potentials, and concentrations of NTs( Epinephrine, Acetylcholine, and GABA), and amino acids; blocks sustained high frequency APs in cell culture. Major therapeutic effect via binding to and prolongation of inactivated state of Na channel – leads to decreased opening of channel with repeated stimulation. |
| Primidone (Mysoline) | Same as Phenobarbital. |
| Tigabine (Gabitril) | Inhibits GABA reuptake transporter (mostly GAT-1) thereby increasing extracellular GABA levels in forebrain and hippocampus. |
| Topiramate (Topimax) | Blocks voltage dependant sodium channels, potentiates GABA effects, and inhibits Ca currents. |
| Vigabatrin | Irreversibly inhibits GABA aminotransferase, thereby preventing degradation of GABA and increasing amount of GABA released at synapse. |
G) Pharmacokinetics:
- Drugs can be administered through two main routes – Enteral, and Parenteral.
- Enteral: refers to medications that undergo first pass metabolism; that is, drugs will enter the hepatic portal circulation and be processed by the liver, before entering the general circulation. Includes oral and suppository medications.
- Parenteral: Bypasses hepatic portal circulation and therefore is free from first pass metabolism (and liver processing) before enter the general circulation. Includes IV, and sublingual medications.
- Liver metabolism before entering the general circulation determines how much active drug is available to be taken up by target cells/organs.
- Some drugs are administered as a pro-drug form, and require first pass metabolism to become active. Other drugs have significantly decreased amounts of active form after liver processing.
- Once in the general circulation, chemical factors such as water solubility, determines where in the body the drug distributes to (ie. areas of greater or lesser lipid content), as well as how much of the drug will become bound by plasma proteins.
- Plasma protein bound drugs are inactive, and remain so until they become unbound or free in the circulation
- Therefore, highly soluble drugs will be distributed in areas of the body with more water content (such as the blood stream), while drugs with more lipophilicity will distribute to areas of higher lipid content (such as the brain). A caveat however, is that drugs with very low water solubility will also take longer to distribute throughout the body owing to decreased carrying ability by the blood circulation.
- Once a drug has exerted its activity, then the body must have a means of removing and eliminating the drug
- There are many different possible means for this event to occur
- Some drugs are eliminated from their site of activity by simple diffusion away from their receptors.
- Other drugs are actively broken down by local enzymes or may auto degrade within the circulation.
- Many drugs will re enter the general circulation in one form or another and be carried to the liver.
- Drugs can be further metabolized to active or inactive metabolites via oxidation of the drug and or glucorinidation.
- Once processed, metabolized (and unmetabolized) drugs may be excreted either via the renal system (and into the urine) or via the biliary system (and into feces)
-
- Once in the liver, hepatic enzymatic processing, usually via one or more enzymes of the Cytochrome P450 system, will break down the drug.
-
- Oxidation and glucorinidation serve to inactivate and to increase the solubility of a given drug, allowing for its excretion from the system.
- All of these factors play into determining the active half life of a given drug, which in turn determines its dosing schedule and loading doses
- Some drugs also have an effect on the hepatic CYP 450 system in itself, by either increasing or decreasing its activity.This effect in turn can increase or decrease the half life of other drugs processed by this system as well as a given medications own half life. Hence, drug interactions are common with medications that potentially affect the CYP450 system. This factor is especially important in pediatric populations where variability in the maturity of liver enzymes can vastly affect drug metabolism/elimination
Specific Drug Pharmacokinetics: Circulation / Distribution and Metabolism
| Drug Name | Circulation and Distribution | Metabolism |
| Benzodiazepines | Widely distributed | Metabolized to many active metabolites |
| Carbamazepine (Tegretol) | Volume of distribution about 1L/Kg; 70% binding to plasma protein | Induces hepatic microsomal (CYP450) enzymes, thereby speeding own metabolism, completely metabolized to active and inactive metabolites |
| Divalproex Sodium (Valproic Acid) | 90% plasma protein bound, confined to extracellular water | Slow hepatic clearance |
| Ethosuxamide (Zarontin) | Peak plasma concentration at 3-7 hrs, distributes uniformly throughout body water; does not solvate in fat; not protein bound | Via hydroxylation |
| Gabapentin | Not plasma protein bound | Is not metabolized, does not induce hepatic enzymes |
| Lamotrigine (Lamictal) | Volume of Distribution of 1- 1.4L/kg with 55% plasma protein bound. | Via hepatic CYP450 enzymes |
| Leviteracetam | Peak plasma concentration in 1.3 hours, less than 10% protein binding | Hepatic CYP450 enzymes |
| Phenobarbital | About 45% plasma protein bound, distributes mainly to brain, liver, kidneys | Hepatic CYP450 enzymes |
| Phenytoin, Fosphenytoin(Dilantin) | Highly plasma protein bound, free plasma levels correlate with therapeutic effect; accumulation in brain, liver, muscle, fat | Metabolized by liver to active and eventually inactive metabolites |
| Primidone (Mysoline) | About 70% unbound as free drug | Oxidation to phenobarbital and scission of ring to form other metabolites. Metabolized similar to phenobarbital |
| Tigabine (Gabitril) | Unknown | Unknown |
| Topiramate (Topimax) | 15% plasma protein bound | About 20-50% metabolized with no active metabolites; no enzymatic induction or inhibition |
| Vigabatrin | Unknown | Unknown |
Specific Drug Pharmacokinetics: Half Elimination and Half life
| Drug Name | Elimination | Half life |
| Benzodiazepines | Urine | 20-40 hrs (depending on drug) |
| Carbamazepine (Tegretol) | About 1L/kg/d in urine | Initially 36 hrs, but can decrease with hepatic enzyme induction to less than 20hrs |
| Divalproex Sodium (Valproic Acid) | Dose dependant, renal elimination | 9-18 hrs |
| Ethosuxamide (Zarontin) | Renal | 40 hrs (18-72) |
| Gabapentin | Excreted unchanged in urine | 5 – 8 hrs |
| Lamotrigine (Lamictal) | Urine | 24 hours, may decrease to 13 – 13.5 with other hepatic enzyme inducers |
| Leviteracetam | Renal, 2/3 unchanged | 6-8 hours; however, duration of effect not correlated to half life (efects may last much longer) |
| Phenobarbital | Urine, wither about 25-50% unchanged | 80-100 hours for adults, 60-180 hours for infants (mean of 110) |
| Phenytoin, Fosphenytoin(Dilantin) | Excreted in urine (mostly metabolized, small proportion unchanged) | 12 to 36 hours, with median of 24 |
| Primidone (Mysoline) | Excreted similar to phenobarbital | 6-8 hrs |
| Tigabine (Gabitril) | Unknown | Unknown |
| Topiramate (Topimax) | Mostly unchanged via urine | 20-30 hours |
| Vigabatrin | Unknown | 6-8 hours; however, duration of effect not correlated to half life (efects may last much longer) |
H) Pharmacotherapeutic agents
- Most patients with seizures respond to drug therapy although a small proportion develop intractable symptoms and require invasive therapy (ie. surgery). Monotherapy or the simplest therapy possible is preferred to minimize side effect profile and cross reactivity between medications. For most anti-seizure medications, blood levels correlate closely to therapeutic and pharmacokinetics of medication. However, the therapeutic index is low; toxicity must be watched for with all seizure medications.
- If patient remains seizure free for 2 years, may consider going off medication at physician’s discretion
I) Overview of Seizure Medications:
- Up to 1990s, main anti-seizure medications could be generally classified into 5 main chemical groups: Barbiturates, Hydantoins, Oxazolidineones, succinimides and acetylureas. These 5 classes shared common heterocyclic ring with different substituents; changes in substituent could drastically alter pharmacology / clinical properties
- Exceptions to this classification schema include carbamazepine, valproic acid, benzodiazepine, felbamate, gabapentin, lamotrigine, oxcarbezepine, tigapine, topiramate, vigabatrin, levetiracetam, and other newer anti epileptic medications
- In general, most compounds are only slightly water soluble with good absorption (80-100% in circulation) and little/poor plasma protein binding. They are mainly cleared by hepatic CYP 450 system via conversion to active metabolites and excretion (renal and biliary). Slow plasma clearance leads to long half life (> 12 hr)
J) Specific Pharmaceutical therapies for Different Seizure Types
- Partial Seizures: Use phenytoin or carbamazepine (current standard; however, all newer seizure medications have shown efficacy)
- Generalized Seizures: Use Phenytoin or Carbamazepine; valproate has shown efficacy as well. For Absence seizures, Ethosuxamide is drug of choice, although valproate and clonazepam are also effective. Evidence has shown that lamotrigine or topiramate can also have an effect.
- Myoclonus: Specific syndromes usually treated with valproate; other medications also having shown to be useful include clonazepam, benzodiazapines in general, and levetiracetam. Juvenile Myoclonic epilepsy, a relatively more common congenital seizure disorder, can be worsened by phenytoin or carbamazepine- therefore, valproate is the first line treatment followed by lamotrigine and topiramate.
- Atonic seizures: Generally refractory to pharmaceutical interventions, although some suggestion that valproate or lamotrigine can be benefical. Benzodiazepines have shown conflicting outcomes with improvement in some, and worsening in others. Felbamate has been tried successfully in some patients; ketogenic diets have also shown benefit. Standard treatment for this seizure type is to deal with the primary medical issue and hope that the seizures resolve concurrently.
- Status Epilepticus: For generalized tonic clonic form of Status Epilepticus, IV Benzodiazepine is usually used, commonly Diazepam (01.-0.3 mg/kg); mdazolam (02.mg/kg) and lorazepam ( 0.05 – 0.1 mg/kg) are also used. Phenytoin (10 – 15 mg/kg) or Fosphenytoin (10 – 20 mg/kg) may be used alternatively or in parallel. If initial bolus measures are ineffective in stopping seizures, then continuous infusions of diazepam are usually used (20mg/kg with loading dose of 10-20 mg /kg Phenobarbital) or IV valproic acid (20 mg/kg) is implemented. Should the latter treatments also fail in halting seizure activity, general anesthesia with ventilatory assist and intubation as necessary is utilized.
- Febrile seizures: Most children usually require no treatment for this condition, although rectal diazepam can be administered to abort prolonged seizures. Daily Phenobarbital or Valproic acid can be used prophylactically, although Phenobarbital at the onset of a febrile illness is ineffective owing to the long course required to reach therapeutic levels. Intermittent use of oral diazepam QID has also been shown to have variable efficacy.
- Infantile spasms: In general, conventional anti-epileptics are not used in treatment of infantile spasms. The main therapy includes costicosteroids and ACTH however, Vigabatrin has been show to be somewhat effective.
Commonly used Anti-seizure medications and Clinical Indications
| Drug Name | Clinical Indications |
| Benzodiazapines | Status epilepticus, partial and generalized seizures |
| Carbamazepine (Tegretol) | Partial seizures, also useful for generalized tonic clonic. Also useful in mania, trigeminal neuralgia |
| Divalproex sodium (Valproic Acid/Valproate) | Absence seizures, myoclonic seizures, atonic attacks, bipolar disorder and migraine prophylaxis |
| Ethosuxamide (Zarontin) | Absence seizures |
| Gabapentin | Effective as adjunct or monotherapy against partial seizures and generalized tonic – clonic; also useful for neuropathic pain and neuralgia |
| Lamotrigine (Lamictal) | Some evidence for monotherapy for partial seizures; suggestion for use in absence and myoclonic seizures in pediatric population |
| Leviteracetam | Partial seizures |
| Phenobarbital | Proven efficacy in partial seizures and generalized tonic clonic; anecdotal evidence for use in other types (contraindicated for some seizure types owing to worsening of symptoms) |
| Phenytoin, Fosphenytoin (Dilantin) | Very effective against partial seizures and orimary or secondary generalized primary or secondary seizures |
| Primidone (Mysoline) | Partial seizures, also useful for generalized tonic – clonic. |
| Tigabine (Gabitril) | Adjunct for partial seizure treatment, or can be used as monotherapy in some |
| Topiramate (Topimax) | Effective as monotherapy for partial seizures and generalized tonic-clonic. Also evidence for use in Lennox-Gastaut, West’s syndromes, and absence seizure |
| Vigabatrin | Partial seizures, infantile spasms |
K) Appendix:
Seizure classification
Partial Seizures: seizures that have an observable, localized foci of onset (via EEG or clinical observation). Further subdivided into:
- Simple Partial Seizures: minimal spread of abnormal neural activity with no change in level of consciousness.
- Complex Partial Seizures: local onset, with generalized bilateral distribution of abnormal activity. Most arise from temporal lobe.
- Secondary Generalized Seizure: seizure secondarily generalizes from partial seizure, evolves from partial to generalized tonic-clonic.
Generalized seizures: Seizures that have bilateral distribution of abnormal activity (on EEG) with an no obvious cortical focal origin.
- Generalized tonic-clonic seizure: 15-30s period of tonic rigidity in all extremity followed by period of relaxation; leads to clonic phase. Secondary type preceded by partial seizure/different type of seizure whereas primary type has no precedent. Medical treatment for both primary and secondary generalized seizures same; uses treatment appropriate to treat partial seizures as well.
- Absence: characterized by acute onset and resolution, usually less than 10 seconds and rarely more than 45\seconds; multiple brief staring episodes. Can repeat itself hundreds of times during day. Characterized by 2.5-3.5 hz wave spike pattern on EEG. Patients presenting with postural changes and atypical EEG changes have poorer prognosis and response to treatment
- Myoclonic Jerking: often occurs secondary to generalized seizure, although can also occur as primary presentation; loose category with many subtypes. Treatment varies, although in secondary cases, is aimed at treating primary seizure disorder.
- Atonic Seizures: sudden loss of postural tone. Most commonly seen in children, although can be seen in adults as well, Treatment includes prophylactic safety measures (ie. helmets)
- Infantile spasms: epileptic syndrome, not a seizure type. Usually characterized by brief, recurrent myoclonic jerks of body with sudden flexion/extension of limbs/body (presentation variable). 90% patients present before 1st year, most patients severely developmentally delayed.
Status Epilepticus:
- A seizure lasting a sufficient length of time (30 minutes in most studies) or if seizures occur frequently enough that consciousness does not return between attacks for greater than 30 minutes. This condition is life threatening as to pyrexia, circulatory collapse, worsening of coma, metabolic derangement, etc, can occur with a mortality rate of 5-10%.
Febrile Seizures:
- can have various etiologies including infection or epilepsy triggered by fever. Can also be result of genetic predisposition to rapid increase in body temperature (occurs in 2-4% of children with 50% cases between 6-12 months of age). If seizure is less than 15 minutes in length with generalized motor convulsions and occurring only once in 24 hr period, then they are considered simple. If the seizure has focal features, lasts longer than 15 minutes, occurs greater than once in 24 hour period, or there are pre existing neurologic conditions, then the seizure is considered complex or atypical. Prognosis of simple febrile seizure is excellent.
L) References
1) Lewis D, “Neurology” in Nelson’s Essentials of Pediatrics, 5th Edition (2006), pp 825 – 875. Elsevier Saunders, Philadelphia.
2) Lindsay KM and Bone I, “Epilepsy” in Neurology and Neurosurgery Illustrated, 4th Edition (2004), pp 90 – 103. Churchill Livingstone, Edinburgh.
3) Porter JM and Meldrum MB, “Antiseizure medication” in Pharmacology, 5th Edition (2003). Chapter 24 (online edition). Churchill Livingstone, Edinburgh.
Acknowledgements:
Written by: Albert Tu
Edited by: Anne Marie Jekyll, Pediatric Resident


 (1 votes, average: 4.00 out of 5)
(1 votes, average: 4.00 out of 5)
Principles of pharmacotherapy in neurology.. Tiptop 🙂