Click for pdf: Suspected Foreign Body Ingestion
General Presentation
Background: Of more than 100,000 cases of foreign body ingestion reported each year in the United States, 80% occur in children, with the majority of the foreign body ingestion being accidental. Most often foreign body ingestion occurs in children between ages of six months and three years; reflecting the tendency of small children to use their mouths in exploration of their world. Coins are the most common foreign body ingested by children; others include toys, toy parts, magnets, batteries, safety pins, screws, marbles, bones and food boluses. In countries in Asia, where fish is a food staple, fish bones are most commonly ingested. Fortunately, mortality rates are low, and most foreign bodies pass harmlessly and are eliminated in the stool. Complications include systemic reactions due to allergies to ingested object, gastrointestinal mucosal erosion or perforation, peritonitis, pneumothorax, and production of an aortoenteric fistula.
Pathophysiology: The location of the foreign body ingested is important for determining the appropriate investigations, prognosis and treatment. This is usually categorized anatomically into esophagus and stomach/lower gastrointestinal tract.
Most complications from pediatric foreign body ingestion are due to esophageal impaction, usually at one of the 3 physiological narrowing areas:
1) about 70% at the upper esophageal sphincter or thoracic inlet,
2) about 15% in the mid-esophagus at the level of the aortic notch, and
3) about 15% just above lower esophageal sphincter.
Patients are at an increased risk if they are small, have an underlying esophageal disease such as a stricture, have undergone previous esophageal surgery, or have ingested several coins at one time.
Once the foreign body has reached the stomach in a child with a normal GI tract, it is less likely to lead to complications. However, exceptions include sharp or toxic bodies, objects too large to pass through the pyloric sphincter (greater than 2×6 cm), and more than one magnet which may attract and adhere tightly through the tract leading to obstruction, necrosis of intervening tissues or even the formation of a fistula.
Clinical Symptoms: Children can often be asymptomatic, have transient symptoms, or have vague symptoms which do not immediately suggest foreign body ingestion; therefore, it is important to always keep the possibility of a foreign body in mind.
Questions to ask
- Did you witness the child ingesting a foreign body?
- Did the child report to you that he/she ingested a foreign body?
- Do you know what the foreign body is? (size, shape, identity)
- Do you know when the child ingested the foreign body?
- Have you found the foreign body in the stool already?
- Has the child previously swallowed any objects before?
- Does the child have any other medical illnesses or have had previous surgery?
- Does the child have fever, abdominal pain, or vomiting? If yes, where is the pain? What color, and how much vomit? Any blood in the vomit?
- Has the child had any stools? If so, how many times, what color? We need to be aware of potential GI obstruction
- Is the child having difficulty breathing or showing any signs of airway compromise? If yes, we need to retrieve the object promptly.
| Esophageal Foreign Body Symptoms | Stomach/Lower GI Foreign Body Symptoms |
| Dysphagia | Abdominal distention |
| Food refusal, weight loss | Pain |
| Drooling, gagging | Vomiting |
| Emesis, hematemesis | Hematochezia |
| Foreign body sensation | Unexplained fever |
| Chest pain, sore throat | |
| Stridor, cough | |
| Unexplained fever |
Differential Diagnosis
| Acute appendicitis | Esophageal stricture |
| Disk battery ingestion | Meckel diverticulum |
| Esophagitis | Intussusception |
| Foreign body aspiration | Pyloric stenosis |
| Gastritis | Reactive Airway Disease |
| Peptic Ulcer Disease | Pharyngitis |
| Gastroenteritis | Pneumonia |
| Munchausen syndrome | Psychiatric diseases |
| Gastrointestinal obstruction-large or small bowel | Pneumothorax |
Investigations and Management
a) Physical exam:
- examine airway and breathing – always manage ABCs before continuing
- examine neck for swelling, erythema, crepitus suggesting potential esophageal perforation and requiring surgical consult
- examine chest for stridor or wheezing suggesting lodged esophageal foreign body with tracheal compression
- examine abdomen for small bowel obstruction (auscultate) or perforation (palpate for pain) which requires immediate surgical consult and abdominal imaging
b) Lab studies: children with foreign body ingestion do not usually require lab testing, although they may be indicated if suspect potential infection
c) Imaging studies:
- Single frontal radiograph of neck, chest and entire abdomen to locate the object; this only works if swallowed object is radiopaque
- If the object is below diaphragm, no further radiographs are necessary
- If object is in esophagus, frontal and lateral chest radiographs are necessary to precisely locate and better identify the object
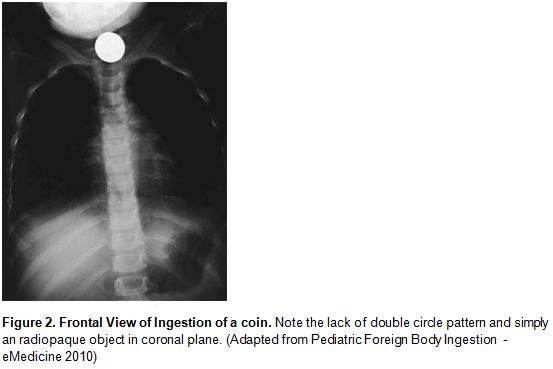
- General rule: if coin is in esophagus, it appears in coronal orientation; if coin is in trachea, it appears in sagittal orientation
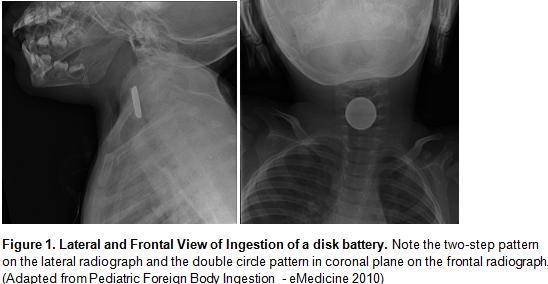
- Coin versus battery: disk batteries have a distinctive two-step profile and a double circle appearance (Figure 1 and 2)
- Endoscopy is preferred over barium contrast studies for radiolucent objects as it allows removal of object as well
d) Metal Detectors: sensitive and specific for identifying the location of ingested metallic objects such as aluminum
e) Endoscopy: children who require extensive radiologic investigation may be referred for endoscopy as it is safe and highly effective
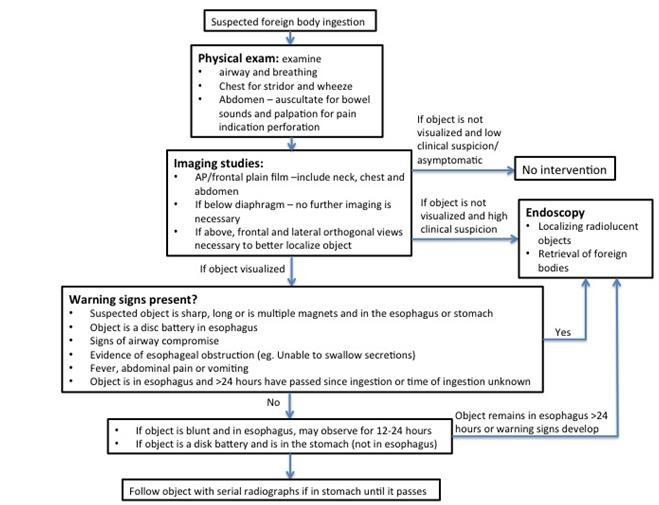
f) Management: see Figure 3 below for management.
(Figure 3 – Management of suspected pediatric esophageal or gastrointestinal foreign body ingestion)
Urgent intervention for:
- When the ingested object is sharp, long (>5 cm), consists of multiple magnets, and is in the esophagus or stomach.
- When a disk battery is in the esophagus (and in some cases in the stomach)
- When the patient shows signs of airway compromise.
- When there is evidence of near-complete esophageal obstruction
- When there are signs or symptoms suggesting inflammation or intestinal obstruction
Approaches for specific types of foreign bodies
a) Coins: usually can be observed for up to 24 hours after ingestion as 20-30% will pass into stomach spontaneously. Esophageal coins should be removed promptly if patient is symptomatic or does not pass esophageous spontaneously by 24 hours after ingestion
b) Disk batteries: a medical emergency, as contact with esophageal wall with both poles of battery can conduct electricity which can rapidly lead to necrosis and perforation of esophagus. However, once passed to stomach, most pass harmlessly.
c) Sharp pointed objects: if lodged in esophagus, represents a medical emergency because 15-35% risk of perforation. Endoscopy should be performed because many sharp pointed objects are not readily visible by x-ray.
d) Magnets: a single ingested magnet is usually low risk, however two or more magnets may attract across layers of bowel leading to necrosis, fistula, perforation or obstruction. Thus, location, and number of ingested magnets are important to determine and multiple magnets ingestion indicates preemptive removal.
References
1) Conners G. Pediatric Foreign Body Ingestion. eMedicine (Last updated July 12, 2010). Available from: http://emedicine.medscape.com/article/801821-overview [Accessed on February 23, 2011]
2) Gilger M, Jain A, McOmber M. Foreign bodies of the esophagus and the gastrointestinal tract in children. (Last updated January 4, 2009) In: UpToDate, Ferry G, Singer J, Hoppin A (Ed), UpToDate, Wellesley, MA, 2010
Kay R, Wyllie R. Pediatric Foreign Bodies and their Management. Current Gastroentereology Reports. 2005; 7: 212-218.
Acknowledgements
Writer: Teresa Liang
Editor: Dianna Louie


 (3 votes, average: 4.33 out of 5)
(3 votes, average: 4.33 out of 5)