Click for pdf: Syncope
1. Definition:
Syncope is defined as a sudden, brief loss of consciousness associated with loss of postural tone from which there is spontaneous recovery. The mechanism of syncopeincludes the brainstem reticular activating system and both cerebral cortices. In most cases syncope is benign, however under certain circumstances cardiac causes of syncope can be life-threatening. In most instances, syncope is simply an individual or familial predisposition to the common faint.
2. General Presentation:
Syncopal events in children are known to most often be benign, however, more serious syncope conditions exist which mainly involvethe cardiovascular system. The following is a list of common conditions, life threatening conditions and other conditions that may present with syncope in children:
Common conditions of syncope:
- Vasovagal syncope – is by far the most common cause of syncope among children. Also known as neurocardiogenic, reflex or the common faint, it typically involves a precipitating event and a prodrome. Precipitating events can include standing or stress (physical or emotional) and even swallowing, hair grooming and micturition. The typical prodrome consists of light headedness, dizziness, nausea, visual changes, pallor and diaphoresis. The mechanism for the common faint involves an exaggerated reflex response in vasomotor tone and heart rate.
- Breath holding spells – are most common in children aged 6 to 24 months. The cause is usually due to an emotional insult such as pain, anger or fear and the child may be cyanotic or pallid. If it is cyanotic, the breath holding begins and cyanosis develops and to loss of consciousness follows. If it is pallid spell, loss of consciousness will occur before breath holding. Breath holding spells sually follow a benign course and are expected to stop by the age of 5. The child may develop vasovagal syncope at a later age.
- Orthostatic hypotension – occurs when there is a sudden reduction in blood pressure greater than 20/10 mm Hg as a result of postural change such as moving quickly from sitting to standing. Dizziness and lightheadedness result. Volume depletion, anemia, and medications can exaggerate this response.
- Toxic exposure – Exposure to toxins can result in decreased cardiac output or loss of consciousness caused by numerous toxins such as barbiturates, tricyclic antidepressants, and phenothiazines. Drugs such as cocaine, alcohol, marijuana, inhalants and opiates can also play a role in toxic exposure leading to syncope some of which can be life threatening.
Life threatening conditions of syncope:
Certain cardiac conditions may present with syncope and can be serious and even life threatening. As a result of either an arrhythmia or structural heart condition, cardiac output may abruptly decrease leading to syncope.
- Primary Electrical Disturbances: In children, usually these are tachyarrythmias. They may be inherited or occur as a result of structural heart disease. Primary electrical disturbances include:
- Long QT syndrome – a disorder of myocardial repolarization characterized by prolongation of QT interval on the electrocardiogram and an increased risk of sudden death due to the potential to degenerate into polymorphic ventricular tachycardia. Long QT syndrome may be acquired or congenital.
- Catecholaminergic polymorphic ventricular tachycardia – is characterized as a electrophysiological disorder that is genetically dictated. Children may present this condition as the result of ventricular tachycardia or ventricular fibrillation caused by emotional or physical stress.
- Preexcitation syndrome – results when the ventricles of the heart depolarize earlier than normal causing a partial premature contraction.
- Congenital short QT syndrome – is a genetically defined disease of the cardia system that involves a short QT interval on the electrocardiogram(< .30 sec) that does not change with heart rate.
- Hypertrophic cardiomyopathy – is the most common cause of sudden death during exercise and occurs when a portion of the myocardium is thickened. It is characterized as a disease of the myocardium that can cause ventricular outflow obstruction, ischemia during exertion and arrhythmia leading to inadequate cardiac output.
- Coronary artery anomalies – This condition occurs when a coronary artery is abnormally located in areas such as between the aorta and pulmonary artery. This can result in the artery being compressed during exercise which can lead to myocardial ischemia and syncope or sudden death.
- Valvar aortic stenosis – causes mild to severe obstruction of left ventricular outflow that may be associated with outer left heart obstructive lesions or extracardiac malformations, including genetic disorders. Current evidence shows that the majority of children with aortic stenosis are asymptomatic, however, sudden death can occur.
- Dilated cardiomyopathy – Occurs when the heart becomes weakened and enlarged and is enable to pump blood efficiently which ultimately affects the lungs, liver and other systems of the body. Causes include viral myocarditis, severe anemia, and in patients with muscular dystrophy.
- Pulmonary hypertension – Children with pulmonary hypertension, either idiopathic or related to a congenital heart defect with a systemic to pulmonary shunt (Esenmenger syndrome), may experience syncope. Most patients develop exertional dyspnea, however, syncope is an indication of more severe pulmonary hypertension and impaired right heart function.
- Acute myocarditis – is characterized as inflammation of the myocardium and is caused by infection to the heart leading to chest pain, heart failure and/or sudden death. Common viruses include Coxsackie A and B and adenovirus.
Other conditions:
- Hypoglycemia – Commonly noted as a cause of syncope, hypoglycemic individuals report feeling weak, hungry and sweaty as a result of a decrease in blood glucose. The decline in blood glucose leads to agitation, confusion and an altered mental status.
- Arrhythmia‘s – Non life threatening arrhythmia’s can cause rhythm disturbances that are not ventricular in origin and may cause syncope that is non-life threatening.
- Supraventricular tachycardia – Involves rapid rhythm of the heart and occurs at the atria or the AV node. Rapid beating of the heart can result in decreased blood pressure resulting in inadequate cardiac output leading to syncope.
- Bradycardia – Examples of syncope in response to bradycardia include sinus node disease, and congenital and acquired heart block. The heart rate is found to be slower in patients with bradycardia and inadequate to maintain a optimal cardiac output which results in the development of syncope.
3. Differential Diagnosis
Many conditions mimic syncope and a thorough history and physical examination will help distinguish which episodes are truly syncopal in nature.
- Seizures – Characterized by a loss of consciousness and postural tone. Seizures will sustain for longer than syncopic episodes and involve aura, prolonged tonic clonic activity, and/or the presence of a postictal phase.
- Migraine syndromes – Can be similar to syncope in regards to loss of consciousness, ataxia, or vertigo. Differences can be distinguished because loss of consciousness concerning migraine syndromes is longer. Further, individuals with migraine syndromes experience neurologic symptoms, headaches and nausea.
- Hysteria/conversion disorder – Most commonly noticed in the presence of an audience, this condition lacks hemodynamic or autonomic changes that can be prolonged however rarely result in injury. Mainly occurs in adolescents.
- Hyperventilation – Correlated with emotional stress, individuals experience chest pain, chest tightness and shortness of breath. Further symptoms include lightheadedness, paresthesias and visual disturbances. Most common in adolescents.
- Choking – Can ultimately lead to death, individuals who participate in self-strangulation or strangulation by another person will experience a euphoric state caused by cerebral hypoxia. Failure to release pressure before loss of consciousness can lead to death.
4. Questions to ask:
Good history taking is very important in order to determine the circumstances associated with loss of consciousness. A good history can help determine whether the event is life-threatening or not. It is also important to determine if the event in fact was a syncopal episode or something else. A thorough history of events surrounding the episode can make it easier to determine if the cause is neurocardiogenic or if other factors are involved. The following, adapted from Grubb and Olschansky (2005) are red flags when trying to determine the etiology of the syncopal episode.:
Conditions that warrant more detailed evaluation of syncope. Adapted from Grubb and Olshansky 2005.
| 1 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Important aspects of the history include:
- Precipitating events, for example:
- Did it occur during physical activity (more concerning for cardiac etiology)
- Did it occur during long periods of standing (more consistent with vasovagal)
- Is it recurrent?
- Any triggers or stressors?
- Description of the episode itself, for example:
- Symptoms of dizziness, visual changes, nausea (vasovagal)
- Abnormal movements (may be indicative of seizure activity)
- Medical history
- A past history of cardiac conditions should immediately increase your concern for cardiac cause of syncope.
- Medications
- Family history
- Sudden death, known arrhythmias, cardiomypathies
5. Physical examination:
Individuals with vasovagal syncope are found to have a normal physical examination, however, a complete cardiovascular physical examination is always warranted as if the condition is cardiac it can be life threatening.
A complete physical examination should be performed including orthostatic vital signs with focus on both cardiovascular and neurologic exams. Cardiac exam may reveal various mumurs if there is an underlying cardiac condition. One should also may close attention for signs of congestive heart failure such as a gallop or hepatomegaly.
6. Investigations:
The history and physical exam should guide whether further diagnostic studies are warranted. Important tests include ECG, glucoometer, CBC (to look for anemia), and urine beta-HCG in a young post-menarchal female.The following flow chart, adapted from Strickberger et al. (2007) will help you determine the extent of syncope and distinguish if the condition is life threatening (cardiac) or not:
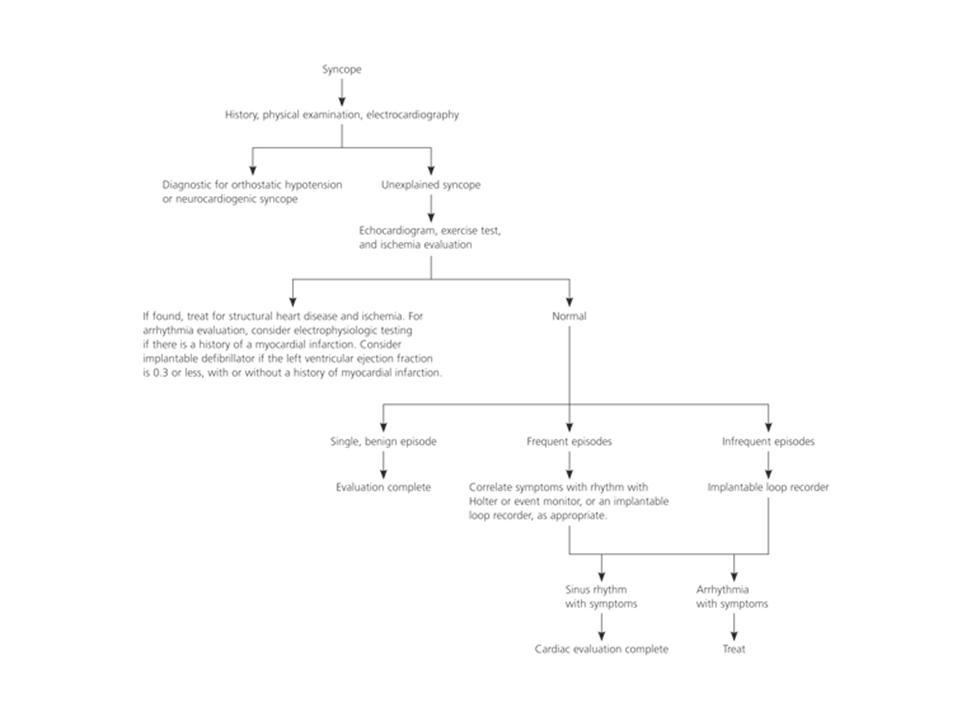
Figure 1: Diagnostic approach to the patient with syncope. Adapted from Strickberger et al, 2007.
7. Conclusion:
Syncope can be a dramatic event that results in loss of consciousness associated with loss of postural tone which can occur spontaneously. Current evidence shows most syncopal events in children are often benign. It is important to acknowledge the severe effects of syncope that are mainly related to cardiac conditions which can lead to sudden death. Generally, recovery from syncope can be resolved within minutes to hours.
References:
Grubb, B. Olshansky, B. Syncope: Mechanisms and Management. 2nd Ed. Blackwell publishing 2005.
Coleman, B. Salerno, J. Causes of syncope in children and adolescents. Uptodate 2008. www.uptodate.com
Horenstein, S. Hamilton, R. 2008. Syncope. Retrieved December 19th 2008 from http://emedicine.medscape.com/article/892358-overview
Strickberger A. Benson, W. Biaggioni, I. Callans, D. Cohen, M. Ellenbogen, K. Epstein, A. Friedman, P. Goldberger, J. Heidenreich, P. Klein, G. Knight, B. Morillo, C. Myeburg, R. Sila, C. Practice Guidelines: AHA/ACCF Statement on the evaluation of syncope. Circulation: Journal of the American Heart Association. January 2007. 113: 316-327
Coleman, B. Salerno, J. Emergent evaluation of syncope in children and adolescents. Uptodate 2008. www.uptodate.com.
Acknowledgements:
Written by John Hilhorst
Edited by Anne Marie Jekyll


 (35 votes, average: 4.40 out of 5)
(35 votes, average: 4.40 out of 5)