Click for pdf: Breastfeeding problems
Introduction
Breastfeeding has been recognized as the optimal sole source of nutrition in infants by the American Academy of Pediatrics. It has many benefits to both infant and mother. Exclusive breastfeeding is recommended in the first 6 months of life and partial breastfeeding (breastfeeding plus introduction of solid foods) for up to at least 12 months of age.
Advantages of breastfeeding to the infant include decreased incidence or severity of diarrhea, respiratory illness and otitis media as well passing protective antobodies (IgE) to the infant. Advantages to the mother include decreased risk of postpartum hemorrhage, longer period of amenorrhea, and reduced risk of ovarian and premenopausal breast cancers. There is also an economic advantage to both mothers and society.
Despite the advantages of breastfeeding, may women choose not to breastfeed for a variety of reasons. Others initiate breastfeeding but stop due to problems that arise. Below, the common problems associated with breastfeeding and their management will be discussed.
General Presentation
Breastfeeding problems are common among mothers and can be very challenging for both the mother and infant. The anxiety that accompanies first-time mothers breastfeeding in addition to underestimated intensity of newborn care can contribute to breastfeeding difficulties. There are many complications associated with breastfeeding which include engorgement, breast tenderness, sore or painful nipples, plugged ducts, and infection of the breast (mastitis).
Effective breastfeeding can often be determined by an infant’s stool. An infant who is successfully breastfed will clear meconium within 3 days postpartum. Delayed clearance of meconium may indicate failure of lactogenesis (milk production), poor latching or ineffective milk transfer. By day 5 of life, the stools should be yellow and seedy. (*Failure to pass meconium within 48 hours is abnormal and the infant should be seen by a physician immediately*)
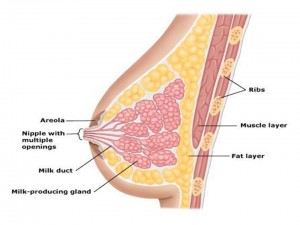
Anatomy:
Figure1: Anatomy of the breast – Adapted from Hopkinson et al. 2008.
Common Breastfeeding problems:
Engorgement:
As one of the most common causes of lactation failure, symptoms of engorgement consist of swelling within the breast tissue. This is most common on the third postpartum day at the onset of large quantities of milk production. The breasts become firm, warm, painful and throbbing and the nipples become nonprotractile. Temperature increases in some women. If severe engorgement occurs, the rigidity of the areola may prevent the infant from latching (tight seal of the infant’s lip around the nipple).. Engorgement may occur early (24-72 hours postpartum) or late in the post-partum period. Early engorgement results from a combination of edema, tissue swelling and milk production whereas engorgement that occurs later is usually strictly due to accumulated milk.
- Management:
- Enhancement of milk flow is key to both preventing and treating engorgement; this starts with a proper latch. Poor latching can result in the infant’s inability to empty the breast. A lactation consult can be very helpful.
- Empty the breasts frequently and completely by breastfeeding
- Expression of milk by hand or breast pump in between feedings to soften the areola and allow the baby to latch on more easily.
- Cold pack or showers can assist in relieving discomfort of engorgement. Heat is not recommended as it will increase tissue swelling, however, it can be used just before breast feeding to improve the flow of milk.
- Massaging the breast gently before feeding can improve milk flow and soften the breast.
- Reverse pressure softening is another technique that is recommended to relive swelling of the nipple making it easier for the infant to latch on to the nipple.
- Mild analgesics (acetaminophen, ibuprofen) may be effective for pain management and are safe in breastfeeding
Sore or Painful Nipples:
Nipples normally are more sensitive during pregnancy and become the most sensitive approximately 4 days after delivery. Soreness is expected within the first 30 to 60 seconds of breast feeding but then improves. However, pain which continues or increases throughout breastfeeding represents trauma. Nipple cracking, bruising or blistering can develop if the infant latches on incorrectly or does not engulf a large enough portion of the area behind the nipple. Overtime, cracking, bruising or blistering can worsen without proper treatment. Pain that continues beyond the first postpartum week is usually represents tissue damage and proper cleaning and care should be applied to the affected area to prevent infection
- Management:
- The keys to painful nipples are a good latch and proper suckling and a lactation consultant may be extremely helpful
- Saline rinse: sore nipples can be rinsed with warm water or a salt water solution and made fresh upon each use to avoid bacterial growth.
- Nipple ointment: APNO (all purpose nipple ointment) can be used to apply a thin layer to the nipples after feeding and it does not need to be wiped off before nursing.
- Moist healing: A purified lanolin or hydrogel dressing can be applied after feeding which gives moisture to the nipples to assist in healing. It is not necessary to remove the lanolin before feeding, however hydrogel dressings must be removed before nursing.
- Other supportive measures including nursing for a shorter period of time, air drying the nipples well after breastfeeding, and beginning feedings on the less sore breast
- Temporary pumping may be necessary as it is better tolerated
Other Common causes of sore or painful nipples:
- Anklyoglossia : Anklyoglossia, otherwise known as tongue tie, is a condition in which the infants’ have a short frenulum which can limit their ability to extend the tongue and compress the milk ducts. Consequently, the infant is not able to latch on to the nipple correctly which can ultimately cause injury to the nipple area of the breast, and prevent the infant from consuming enough milk. However, anklyoglossia is a very common condition and the major of infants are able to breastfeed without difficulty.
- Treatment of Anklyoglossia:
- Anklyoglossia which is severely affecting breastfeeding can be treated with a procedure called a frenotomy, which releases the short frenulum and improves the ability for the infant to latch on properly and prevent nipple soreness for the mother. Infants are able to breastfeed immediately after the procedure.
- Yeast Infections: These infections are characterized by burning nipple pain, red or itchy nipples, or shooting pains deep in the breast.They are most commonly caused by candida albicans. If the nipple is already injured (cracked, bruised, etc.) then the possibility of yeast infection is increased and the risk of passing a yeast infection onto the infant is a high possibility. Thus, it is important to look for a yeast infection in the infant’s mouth, also known as thrush, and to treat both the infant and mother.
- Treatment for yeast infection:
- Infants can be treated with Nystatin (an antifungal medication) which can be applied to the cheeks and tongue with a cotton swab or small syringe. The mother can be treated with an antifungal cream, such as Miconazole, or an oral medications such as fluconazole (Diflucan). Reoccurrence is very common among mother and infant with yeast infections and all potential sources of re-infection must be removed (ex. pacifier, bottles, toys etc.). Objects that come in contact with the infant’s mouth should be treated with boiling hot water daily and replaced at the end of each week. As for the mother, bras, and clothing that comes into contact with the infected breasts should be washed in hot water and dried in high heat or the sun.
- Treatment for yeast infection:
- Plugged Ducts: Areas in the breast in which plugs of skin and milk block the flow of milk and result in mammary distention. Often there is a palpable breast lump and localized tenderness. They are distinguished from mastitis by the absence of systemic signs of infection. The etiology is unknown, but predisposing factors are similar to that of engorgement including abundant milk supply, poor latching and inadequate emptying of the breast. Plugged ducts which persist may result in galactoceles also known as milk retention cysts which will eventually get resorbed.
- Management:
- Plugged ducts are best treated by completely emptying the infected breast frequently. Breastfeeding with the affected breast will assist in fully emptying the breast and is best done by placing the infant with the nose pointed toward the plugged area which can assist in drainage of milk. Further treatment can include massaging and warm showers as well as rest which promote milk release. It is important to contact a physician if the problem persists for more than 72 hours as definitive treatment is likely necessary
- Definitive treatment include both ultrasound and aspiration.
- Management:
- Mastitis: An infection of the breast in which areas of the breast become hard, red, tender and swollen. Other symptoms that accompany mastitis include systemic signs of infection such fever, muscle aches, chills and general malaise. Common causes of mastitis include Staphylococcus aureus, Streptococcus species and Escheria coli. Left untreated, mastitis may develop into a breast abscess.
- Management:
- Continued frequent nursing with complete emptying
- Antibiotics to treat the infection, most commonly dicloxacillin or cloxacillin for 10 to 14 days
- Supportive measures such as analgesics (ie. ibuprofen) to relieve pain.
- Plenty of rest and massaging the affected breast during nursing can also help prevent discomfort.
- If a breast abscess develops, antibiotics and drainage are necessary; drainage can be accomplished by needle aspiration or an incision and drainage if aspiration fails.
- Management:
- Bloody Nipple Discharge: Although rare, some women have bloody nipple discharge soon after delivery. Blood vessels in the breast ducts during pregnancy increase and are the main cause of bloody nipple discharge which appears as bright red colostrum. It is not necessary to stop nursing if blood is seen in the breast milk. Bloody nipple discharge can be detected in the breast milk or in the infants stool.
- Management:
- The usual cause of bloody nipple discharge can be a result of misuse of breast pumps and cracked nipples. Thus, modification to the breast pump may be needed. If there are no obvious sources causing bloody nipple discharge, a milk specimen must be taken in order to determine if it is a cancerous issue.
- Management:
- Overactive Milk Ejection Reflex: Rapid ejection of milk may be the result of copious milk production. This occurs when milk production increases rapidly between three to four days after delivery until approximately two to four weeks postpartum. When milk production increases too rapidly, milk ejection occurs too quickly making it difficult for the infant to swallow; resulting in the infant coughing and/or gagging.
- Management:
- Nurse the infant in a semi-upright position and allow the infant to interrupt nursing frequently.
- Reduce the flow of milk by gently compressing the base of the nipple during the first several minutes of nursing to slow the initial milk flow.
- Hand express until the initial let-down occurs and then allow the baby to latch onto the breast.
- Nurse frequently to minimize the amount of milk that collects. Having less milk collected in the breasts will reduce the force of milk flow.
- Use a nipple shield to create a reservoir for the milk.
- Management:
- Nipple Colour Changes: Colour changes result from the constriction of the blood vessels of the nipple can cause the nipple to become painful and whitened during, immediately after, and between feedings. This condition is commonly seen in women who have the Raynaud phenomenon or unusual cold sensitivity. Some women have a two part color change (white and blue) or the classic three color change (white, blue and red).
- Management:
- It is important to alleviate blood vessel constriction. Four ways to do this are:
- Increase the air temperature and wear warm clothing.
- Apply a warm compress just before and after nursing.
- Discontinue use of tobacco products
- Avoid medications that constrict blood vessels if possible.
- Management:
- Biting :Teeth begin to show in infants by six to ten months of age. The small sharp teeth can cause injury and/or pain to the nipple which can ultimately affect the function of the nipple.
- Management:
- As soon as biting begins immediately remove infant from the breast and offer a teething toy. It is important for the mother to keep a close eye on biting and once the behavior is noticed bring the baby more deeply onto the breast to prevent biting.
- Another technique is to give the infant a cold teething ring or cloth to suck on before nursing which will make the infant more comftorable and less likely to bite.
- Management:
Conclusion
Breastfeeding problems are seen regularly in mothers and most problems are easily managed with many treatment options available. Lactation consultants are extremely helpful and are recommended for all mothers with breastfeeding problems. It is also important to remember that first time mothers may have significant anxiety around breastfeeding that is contributing to their difficulties. Early detection and a treatment plan are optimal to improve the infants breastfeeding experience and prevent infection of the breast.
References:
1. Hopkinson J, Schanler RJ. Common breastfeeding problems. Up To Date 2009. www.uptodate.com.
2. Hopkinson J, Schanler RJ. Breastfeeding in the perinatal period. Up To Date 2009. www.uptodate.com.
3. Royal college of midwives. Successful breastfeeding: Third Edition. Elsevier health sciences 2002.
4. Kleigman RM, Marcdante KJ, Jensen HB, Behrman RE. Nelson Essentials of Pediatrics 5th Edition. Elselvier Saunders, 2006.
Acknowledgments:
Written by John Hilhorst
Edited by Anne Marie Jekyll



We’re a group of volunteers and starting a new scheme in our community. Your web site offered us with valuable info to work on. You’ve done a formidable job and our entire community will be grateful to you.
Excellent post. I was checking continuously this blog and I am impressed! Very helpful info specifically the last part 🙂 I care for such information a lot. I was looking for this certain information for a long time. Thank you and good luck.
I just couldn’t depart your website before suggesting that I really enjoyed the standard info a person provide for your visitors? Is gonna be back often to check up on new posts