Click for pdf: Obesity
General presentation
Obesity occurs in the pediatric population when a child is pathologically above the range of normal weight for his or her age and height.
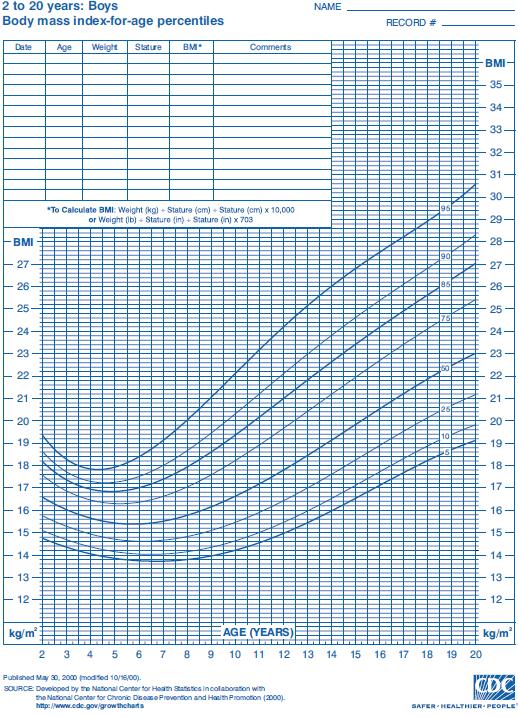
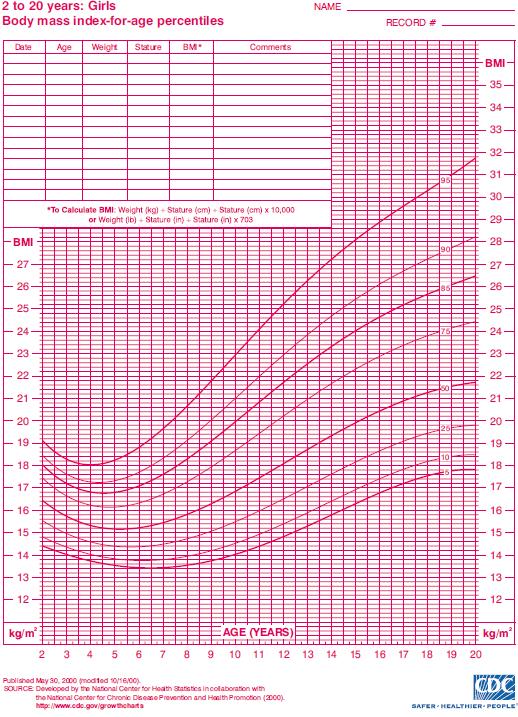
Body mass index (BMI) is calculated as weight (kg) divided by height squared (m2), is used to assess body composition, and correlates closely with the individual’s total body fat from a DEXA scan.
According to the Centers for Disease Control and Prevention, Atlanta, Georgia, overweight children are between the 85th and 95th percentile of BMI-for-age while obese children are above the 95th percentile. BMI-for-age charts are shown for males in Figure 1 and for females in Figure 2. In the United States, for example, about 21-24% of children are overweight and another 16-18% are obese. In Canada, the rate of childhood obesity rose from 11% in the 1980s to 30% in the 1990s. While genetics and hormonal contribute to this statistic, the majority of cases of obesity are due to a decline in the levels of physical activity and increased caloric intake.
The WHO BMI-for-age charts are also commonly used: http://www.who.int/childgrowth/standards/cht_bfa_boys_p_0_5.pdf
http://www.who.int/childgrowth/standards/cht_bfa_girls_p_0_5.pdf
The negative effects on health are both acute and chronic. Children who are obese are predisposed to type 2 diabetes, hypertension, and numerous other cardiovascular risk factors. They also tend to be obese as adults. Childhood obesity may also lead to poor self-esteem, depression, or teasing by peers.
Risk factors for childhood obesity include diet, lack of exercise, family history, psychological factors (stress, boredom, etc), family factors, and socioeconomic factors.
Questions to ask the child/parent
- Do a complete history including HPI, past medical history, medications, family history, development, immunizations, allergies and social history. For an adolescent include a HEADS assessment.
- Specific questions to ask include:
- What does he/she eat in a typical day? Per meal? Portion size? (get them to show you the size of their plate and how much of their meal is carbohydrates/fats/protein/dairy) Snacks outside of mealtimes? Frequency of fast food? How often does the family eat dinner together? Where do they eat dinner – at the table or in front of the TV?
- How many minutes/ hours of physical activity does he/she participate in during a typical day? At school? After school? Weekends?
- How many combined minutes/ hours in a typical day does he/she watch TV, use the computer, or do a sedentary activity? Afterschool? Weekends?
- Can the parent offer some ideas as to what can be affecting the child’s weight? How long has this been going on for?
- How does weight affect the child’s daily function? Is he/ she being bullied?
- Ask about any history of psychological problems such as eating disorders, eating to cope with problems, or depression.
- How does he/she feel about how he/she looks?
- Does he/she have any diagnosed medical conditions? Is he/she on any medications?
- Does he/she have any family members with weight problems?
- Does he/she and the family feel ready to make lifestyle changes?
- Has he/she tried any diets/ regimens to try to lose weight?
Differential diagnosis
- Imbalance of energy intake and expenditure
- Inadequate physical activity
- Factors influencing physical activity:
- Social: e.g. having higher socioeconomic status or more active friends tend to be more active themselves
- Cultural & ethnic: e.g. differences in levels of spontaneous physical activity exist
- Gender-specific: e.g. boys tend to be more active than girls
- Environmental: e.g. electronics promoting sedentary behaviour, or lack of/ no access to community spaces for activities
- Familial: e.g. parents who are overweight or more sedentary tend to have children who are also overweight and less active
- Hormonal dysfunction, e.g.
- Hypothyroidism
- Growth hormone deficiency/ resistance
- Polycystic ovarian syndrome
- Genetic syndromes, e.g.
- Praeder-Willi syndrome
- Cushing syndrome
- Laurence-Moon-Biedl (Bardet-Biedl) syndrome
- Medications, e.g.
- Cortisol, glucocorticoids, insulin, antipsychotics, etc.
Investigations
Physical
- Physical exam, including assessment of vital signs
- Weight and height taken with the patient dressed in a hospital gown, to calculate BMI
- Comparison of patient’s BMI with diagnostic criteria and recording on a growth chart
- Waist circumference
- Examine for cushingoid facies, acanthosis nigracans, striae, and a buffalo hump.
Laboratory
- Lipids, cholesterol
- Fasting blood glucose
- Specific hormone levels to rule out metabolic/hormonal causes of obesity (e.g. autoimmune thyroid disease, polycystic ovarian syndrome, Cushing’s syndrome, etc).
Other
- Physical activity screening tools such as the World Health Organization Health Behaviour in Schoolchildren (WHO HBSC) or the International Physical Activity Questionnaire (IPAQ).
Prevention and treatment
All children older than two years should have their height and weight measured and their BMI calculated at least yearly.
Children and adolescents should perform 60 minutes (1 hour) or more of physical activity each day. Aerobic activity should make up the majority of the 60 minutes. Examples of aerobic activity include brisk walking, running, and swimming. Muscle strengthening activities should be performed at least 3 days per week. Examples of muscle strengthening activities include gymnastics, and push-ups. Bone strengthening activities should also be performed at least 3 times per week. Examples include jumping rope and running.
American Academy of Pediatrics Recommendations:
- Prevention: For all patients, and should include promotion and support for breastfeeding, family meals, limited screen time, regular physical activity and yearly BMI monitoring. Encourage the families to focus on creating a home environment that supports healthy choices.
- Prevention Plus: For children between the 85th – 94th percentiles BMI. Specifically encourage 5 servings of fruits and vegetables/day, 2 hours or less of screen time, 1 hour or more of physical activity and no sugared drinks. Also discuss the importance of family meal time, limiting eating out, consuming a healthy breakfast, preparing your own foods, and promotion of breastfeeding.
- Structured Weight Management: Used if prevention plus has not been effective and BMI is between 95th – 98th percentiles. This approach combines more frequent follow-up with written diet and exercise plans.
- Comprehensive Multidisciplinary Intervention: Used when 3 – 6 months of structured weight management has failed to achieve targets. This approach combines more frequent visits with an MD and a dietician and could also include exercise and behavioural specialists.
- Tertiary Care Intervention: For patients with BMI 99th percentile or greater and with associated comorbidities or for those who structured weight management and comprehensive multidisciplinary intervention were not effective. This approach consists of all that is contained in the previous delivered interventions plus consideration of more aggressive therapies including meal replacements, pharmacotherapy, and even bariatric surgery in selected adolescents.
Treatment for children under age 7 with no other health concerns is weight maintenance rather than weight loss. Allowing the child to gain height but not weight will cause BMI to drop over time into a healthy range.
Weight loss is recommended for children over age 7 or for younger children with related health concerns. Weight loss regimes should consist of a combination of healthy eating and adequate physical activity.
Orlistat (Xenical) is a prescription weight-loss drug approved for adolescents older than 12. It prevents the absorption of fat in the intestines. Prescription weight-loss medication isn’t often recommended for adolescents, due to the unknown long-term risks of the medications, and the fact that a prescription drug doesn’t replace the need to adopt a healthy diet and exercise regimen.
Weight-loss surgery is an option for severely obese adolescents in whom conventional weight-loss methods have failed. However, the long-term effects of weight-loss surgery on a child’s future development and growth are not well known.
References
South-Paul JE, Matheny SC, Lewis EL. CURRENT Diagnosis & Treatment in Family Medicine. 3rd ed. New York: McGraw-Hill Companies Inc; 2011.
Schwarz SM, Freemark M. Obesity [Internet]. 2010 [updated 2010 Oct 8; cited 2011 Jan 04]. Available from: http://emedicine.medscape.com/article/985333-overview
Mayo Clinic. Childhood Obesity [Internet]. 2010 [updated 2010 Oct 9; cited 2011 Jan 04]. Available from: http://www.mayoclinic.com/print/childhood-obesity/DS00698/METHOD=print&DSECTION=all
Centers for Disease Control and Prevention. Clinical Growth Charts [Internet]. 2009 [updated 2009 Aug 4; cited 2011 Jan 04]. Available from: http://www.cdc.gov/growthcharts/clinical_charts.htm
Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. AU Barlow SE, Expert Committee. SO Pediatrics. 2007;120 Suppl 4:S164.
Acknowledgements
Written by: Jackson Chu, Charlie Zhang
Edited by: Dianna Louie


 (6 votes, average: 4.67 out of 5)
(6 votes, average: 4.67 out of 5)