Click for pdf: Neonatal Jaundice
Background
The term “jaundice” comes from the root jaune, the French word for “yellow”. Jaundice is common in the neonatal period, affecting 50-60% of newborns. Jaundice is not a disease by itself, but rather, a sign that results from hyperbilirubinemia, the excessive accumulation of bilirubin in the blood. Hyperbilirubinemia at high levels can however have toxic effects on the body, such as kernicterus.
There are two main types of hyperbilirubinemia:
- Unconjugated / indirect hyperbilirubinemia – can be physiologic or pathologic
- Conjugated / direct hyperbilirubinemia – always pathologic
Basic Physiology
Bilirubin is a bile pigment that is formed from the breakdown of heme, mainly as a product of red blood cell degradation. Unconjugated bilirubin is not very soluble in aqueous solution, and therefore needs to be bound to albumin in the blood. The conjugation process takes place in the liver, and produces a water-soluble conjugated bilirubin, which is ready to be excreted from the body.
Jaundice is visible when serum bilirubin levels are greater than 85-120 umol/L and tends to be more severe or prolonged with prematurity, acidosis, hypoalbuminemia and dehydration.
Questions to Ask
- History of Present Illness
- Onset and progression of jaundiced skin
- Feeding: breast milk or formula?
- Current weight compared to birth weight. Gaining weight appropriately?
- Number of wet diapers per day? (Indicator of hydration status)
- Consistency and colour of stool?(pale stool implies poor bili excretion)
- Infections or fever?
- Medications? (newborn or mother)
- General activity: irritable? lethargic?
- Gender & ethnicity? (Males, Asians, and Blacks have some increased risk
- Perinatal History
- Maternal blood group
- Maternal illnesses or infections
- Results of antenatal screening tests
- Maternal medicine or drug intake
- Delayed cord clamping (could indicate polycythemia)
- Birth trauma with bruising
- Results of newborn screening tests
- Family History:
- Previous siblings with neonatal jaundice
- Other family members with jaundice
- Anemia or blood disorders
- Splenectomy
- Bile stones or gallbladder removal
Differential diagnosis
There are numerous causes of jaundice in a neonate, organized into those which result in an unconjugated (indirect) hyperbilirubinemia or a conjugated (direct) hyperbilirubinemia.
- Unconjugated:
- Polycythemia
- Hypothyroidism
- Sepsis
- Isoimmunization (ABO incompatibility, Rh Disease, other)
- Prematurity
- Physiologic
- Birth trauma/bruising
- Red cell enzyme or membrane defect (G6PD, Spherocytosis, elliptocytosis, phosphokinase deficiency)
- Hemoglobinopathy (sickle cell, thalessemia)
- Conjugation defects (Crigler-Najar, Gilberts)
- Inborn errors of metabolism
- Breast feeding associated jaundice
- Conjugated (almost always pathologic):
- Biliary atresia
- Congenital abnormality of the biliary tree
- Viral Infection (TORCH infections)
- Sepsis
- Hepatitis (multiple causes)
- Long term TPN
- Inborn errors of metabolism
- Alfa-1 antitrypsin deficiency
- Cystic fibrosis
Physical examination
- The jaundiced neonate requires a full physical examination with emphasis on the following:
- General: Does the child look well or unwell? You may be able to observe the child feeding – is the baby having difficulty feeding? Is the baby consolable?
- Vitals: If febrile, the newborn will require a full septic work-up. In hemolytic states, there can be an increase in heart rate and respiration rate as well as poor perfusion.
- Growth Parameters: Obtain length, weight and head circumference and compare to measurements taken at birth. Depending on the newborn’s age, excessive weight loss or insufficient weight gain may point to dehydration.
- HEENT: Is there pallor? Sclerae and mucous membranes should be closely inspected for jaundice. Look for cephalohematoma or bruising. Remember that jaundice first becomes clinically apparent at the cephalic end of the body, and only progresses caudally as serum levels increase.
- Cardiovascular: Heart rate, pulse volume, blood pressure, apex location, perfusion. Severe haemolytic processes can result in heart failure.
- Respiratory: Respiration rate and rhythm and oxygen saturation. If the neonate is in heart failure, there may be respiratory signs.
- Abdomen: Is the abdomen distended? Is there caput medusa (evidence of portal hypertension)? Are there any masses? Check for hepatomegaly and splenomegaly. Are there any areas of tenderness?
- Neurologic: Level of consciousness. Cranial nerves, tone, gross motor movements, quality of the cry, and primitive reflexes (Moro, grasps, tonic-neck, step).
Investigations
- Hemolytic work-up
- Serum bilirubin: conjugated and unconjugated
- CBC (mainly for Hb and Hct but also WBC as a non-specific marker of infection)
- Peripheral blood smear (for RBC morphology)
- Maternal blood group and Rh status
- Infant blood group and Rh status
- Coomb’s test
- Also consider:
- Septic work-up if clinically indicated
- G6PD (Glucose-6-Phosphate Dehydrogenase) screen (especially if male and of Asian or Middle Eastern ethnicity)
- Other red cell enzyme studies if hemolysis remains undefined
- Liver enzymes (AST, ALT, GGT, Alk Phos) and liver function tests (PT, PTT, albumin, ammonia) if conjugated hyperbilirubinemia
- Imaging studies
- consider abdominal Ultrasound if conjugated hyperbilirubinemia
Treatment
The goal is to prevent kernicterus. Breast feeding does not need to be discontinued. The underlying cause should be treated if possible (i.e. correct dehydration, treat sepsis). The main treatment modalities include phototherapy (blue light, 420-470 nm wavelength) and if needed, exchange transfusions.
Appendix
Bilirubin Measurements
The van den Bergh reaction is the most commonly used test to detect bilirubin in a blood sample. In this reaction, the bilirubin combines with a specific acid reagent to form coloured pyrroles.
- Total bilirubin represents all bilirubin which will react to form coloured pyrroles .
- Direct or conjugated bilirubin is that which reacts with the acid reagent in an aqueous medium. It is water-soluble.
- Indirect or unconjugated bilirubin is obtained indirectly. It is calculated simply by subtracting the direct measured fraction from the total bilirubin level
- In some labs, high performance liquid chromatography is used in place of the van den Bergh reaction.
Kernicterus
Kernicterus is a severe neurologic condition associated with very high levels of unconjucated bilirubin in the blood. Characteristically, there is yellow staining in the basal ganglia, which is accompanied by widespread cerebral dysfunction.
Kernicterus is caused by free (unbound, unconjugated) bilirubin that crosses the blood brain barrier and enters brain cells. This can happen when there is hypoalbuminemia, since unconjugated bilirubin binds tightly to albumin in the blood, or drugs in the bloodstream that displace bilirubin from the albumin binding spots (such as sulfa drugs). Also, in conditions like sepsis, asphyxia and acidosis, the blood-brain barrier is more susceptible to penetration.
Symptoms of kernicterus can be severe and include: lethargy, irritability, hypotonia, opisthotonos, seizures, mental retardation, and hearing loss.
Phototherapy:
The main purpose of phototherapy is to convert unconjugated bilirubin into a form that is easily excreted by the body, thereby prevent the complications of unconjugated hyperbilirubinemia. The jaundiced newborn is placed under blue light (420-470 nm). The unconjugated bilirubin in the baby’s skin will absorb light at this wavelength and will undergo a photoisomerization reaction to be converted into an isomer that can be excreted without the need for conjugation.
Important notes about phototherapy:
- Serum bilirubin should be monitored during and immediately after therapy because there is a risk of rebound since the photoisomerization is reversible when the light is removed.
- Phototherapy is contraindicated in conjugated hyperbilirubinemia (it will result in a “bronzed baby”).
- Side Effects:
- Hypernatremic dehydration (increased insensible losses due to skin surface area exposure) – adjust maintenance fluids accordingly
- Eye damage
- Skin rash
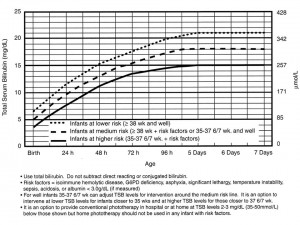
What are the guidelines for phototherapy?
Exchange Transfusions:
The main purpose of the exchange transfusion is to prevent toxic effects of bilirubin by removing it from the body. It is indicated for high levels of bilirubin and/or high rates of rise of bilirubin. The technique requires experience.
Large IV lines (often umbilical venous catheterization) are required, and position is confirmed radiologically. Aliquots of the baby’s blood are withdrawn, and replaced with completely cross-matched blood (or, in acute settings type O Rh blood can be used) warmed to 37oC. Most of the significant complications of exchange transfusions are related to placement of the umbilical lines, which is why special care must be taken with this procedure. Other complications are rare and are related to transfusion reactions.
References
Andreoli, T. E. et al. Cecil Essentials of Medicine, 6th Ed. W.B. Saunders Company. 2004.
Dixit, R and L.M. Gartner. The jaundiced newborn: Minimizing the risks. Original Source: Contemporary Pediatrics, Published April 1, 1999.
Dworkin, P.H. NMS Pediatrics, 4th Ed. Lippincott Williams & Wilkins. 2000.
Hansen, T.W.R. Neonatal Jaundice. Emedicine.com.
Ipp, M. Jaundice and dehydration in the early discharaged healthy term newborn
Kliegman, R.M. et al. Nelson’s Essentials of Pediatrics, 5th Ed. Elsevier. 2006.
Lewis, D. A. and J.J. Nocton. On Call Pediatrics. W.B. Saunders Company. 1997
Molckovsky, A. and K.S. Pirzada (Eds). The Toronto Notes. Toronto Notes Medical Publishing Inc. 2004.
Porter, M. Hyperbilirubinemia in the term newborn. American Family Physician, 2002.
Subcomittee on Hyperbilirubinemia. Management of Hyperbilirubinemia in the Newborn Infant 35 or More Weeks of Gestation. Pediatrics, 2004. 114: 297-316. available online at http://www.pediatrics.org/cgi/content/full/114/1/297
Acknowledgements
Written by: Gina Gill
Edited by: Jeff Bishop


 (38 votes, average: 4.21 out of 5, rated)
(38 votes, average: 4.21 out of 5, rated)