Click for pdf: Fever in the newborn period
Definitions
Fever is defined as a core body temperature greater than 38°C (100.4°F) in infants younger than 28 days and greater than 38.2°C in infants older than 1 month. Core body temperature is best estimated by rectal temperature.
Fever is an extremely common pediatric presentation and has many different causes. Fever is not an illness but rather a sign. The physician’s job is to attempt to diagnose the cause of the fever and to determine if that cause requires treatment or not.
It is important to note that the pattern of fever varies depending on both the age of the child and the nature of the illness. Neonates, for example, may have a hypothermic response to an infection whereas slightly older children may respond to an infection with an extremely high fever (temperatures > 40°C).
Febrile illnesses in children are most often classified as follows:
- Fever of Short Duration: A fever which is accompanied by localizing signs and symptoms that allow the establishment of a diagnosis through an appropriate history and physical. Eg. Fever due to upper respiratory tract infection in a child with a runny nose and cough.
- Fever Without a Focus: This accounts for approximately 20% of febrile children where a fever presents without localizing signs. The history and physical fail to establish a diagnosis.
- Fever of Unknown Origin: A fever lasting for more than 14 days without an identified etiology despite appropriate history, physical, and laboratory investigations or after 1 week of hospitalization and evaluation.
Overview
A thorough history and clinical exam is essential in the evaluation of febrile infants. The most common etiology of fever in infants is a viral infection and include herpes simplex virus, varicella, enteroviruses, influenza virus, respiratory syncytial virus and some adenoviruses. Bacteria that infect infants and cause significant infection include Group B streptococcus, Escherichia coli and Listeria monocytogenes. The common sources of serious bacterial infections are urinary tract infections, bacteremia, osteomyelitis, cellulitis, bacterial gastroenteritis, meningitis, and pneumonia.
Despite the fact that most fevers in infants arise from benign viral infections, you must be able to identify those infants at high risk for serious illness. Once these children are identified, empiric antibiotics should be initiated in order to lessen the chances of serious adverse consequences. Neonates and infants are managed specifically according to their age and risk assessment. They are divided into 2 major categories:
Fever in infants younger than 3 months old:
- Neonates (birth to 28 days)
- Young infants (29 to 90 days)
Fever in older infants and young children (3 to 36 months):
There is a lack of definitive data to guide patient risk assessment and thus each patient must be treated individually. The risk assessment should however, be based upon several factors such as gestational age at birth, previous hospitalizations, rectal temperature and laboratory assessment. The Rochester low-risk criteria for infants less than 3 months of age are described below.
History and physical examination
An important principle to remember is that the younger a child is the more challenging it becomes to clinically assess their degree of illness. Thus, a detailed history is very important and can provide clues to the specific etiology of the fever. Questions should be asked about associated respiratory and gastrointestinal symptoms, changes in feeding patterns, irritability, activity levels and other changes in behaviour. Always clarify the use of the word lethargic; parents and physicians often have very different meanings for the word. Parents tend to use the word lethargy to describe fatigue versus doctors who use lethargy to describe a more serious state wherein the patient is unable to be fully roused. The birth history is also very significant in an infant presenting with fever. Increased risk of vertically transmitted infection is associated with perinatal maternal fever, positive group B streptococcus status without appropriate prophylaxis, maternal sexually transmitted infections and prolonged rupture of membranes. Finally, it is also critical to know if the infant has had any recent exposures to sick contacts, any previous illnesses or antibiotic use.
The physical exam should include vital signs, skin colour, level of alertness, exanthems and hydration status. You must quickly be able to identify a toxic infant who requires immediate management from a non-toxic infant. A toxic neonate or infant may present with irritability, inconsolability, poor tone, decreased activity, lethargy, poor perfusion and abnormal vital signs. The signs and symptoms of specific infections will not be discussed here but it is imperative that physicians are able to recognize signs of localized infections.
Fever in infants less than 3 months old
When fever presents in infants less than 3 months old, management is guided by dividing them again according to age into neonates (age 0-28 days) and young infants (29 to 90 days). It is recommended that ALL neonates who present with a rectal temperature ≥ 38°C be admitted to hospital and receive a full septic workup REGARDLESS of the neonate’s clinical appearance. This consists of a complete blood count (CBC) and differential, blood cultures, a urinalysis for urine cultures and a lumbar puncture for cerebral spinal fluid (CSF) cultures. If the neonate presents with any respiratory signs or symptoms (e.g. nasal flaring, grunting, increased respiratory rate, retractions, stridor) a chest radiograph should be performed. Similarly, if there are any gastrointestinal signs or symptoms such as diarrhea, a stool culture and sensitivity should be obtained. Empiric antibiotic treatment with ampicillin and gentamycin should be initiated. Suspect a CNS or disseminated herpes simplex virus infection if the neonate is lethargic, has mucocutaneous vesicles, seizures, elevated liver transaminase enzymes, a negative CSF gram stain and/or active maternal herpetic infection. In these cases, empiric acyclovir should be initiated.
Young infants aged 29 to 90 days are assessed and managed according to whether they appear ill or not. They are classified as high or low risk of serious bacterial infection according to the Rochester criteria:
|
Low risk |
High Risk |
|
Well appearance |
Toxic clinical appearance |
|
Previously healthy, term infant and hospitalized no longer than the mother |
Abnormal cry |
|
Lack of obvious focal infection |
Temperature ≥ 38.5°C |
|
WBC 5000 – 15000/mm3 |
Fail low risk Rochester criteria |
|
Band count < 1500/ mm3 |
CRP > 5 |
|
Urinalysis normal (<10 WBC/high power field and no bacteria seen) |
|
|
Stool < 5 WBC/high power field (if diarrhea present) |
|
|
CRP < 5 |
Table 1: Rochester criteria for low risk infants. Adapted from Kourtis et al, Clinical Pediatrics 2004. WBC = white blood cells; CRP = C-reactive protein
In this age group, high risk infants are those who appear toxic and those with an abnormal cry and temperatures ≥ 38.5°C. They should all be admitted to hospital and undergo a full septic work up. These infants should be treated empirically with third generation cephalosporins such as ceftriaxone.
Infants between the ages of 29 and 90 days (1-3 months) with a temperature ≥ 38°C who appear well and are categorized as low risk should undergo a complete history and physical in addition to a septic work-up. The lumbar puncture may not be necessary in some well-appearing infants; however, if empiric antibiotics are started, it is suggested that a lumbar puncture be performed. Those infants with an abnormal chest film should be admitted to hospital. Infants with an abnormal urinalysis consistent with a urinary tract infection should also be admitted to the hospital and started on presumptive antibiotics. Well appearing infants in this age group with normal laboratory evaluation and normal chest x-ray can be considered for outpatient management as long as reliable follow-up within 24 hours can be arranged. Treatment with ceftriaxone is recommended for these outpatients. If adequate follow-up is not ensured, a more aggressive work-up and empiric therapy may be indicated.
Fever in infants aged 3 to 36 months:
The majority of children in this age category who present with fever have a self-limited viral infection or a bacterial infection with a recognizable source. Unfortunately, the history and physical examination do not always identify the source of the fever and it becomes classified as a fever without a source. Fever ≥ 39°C is the general threshold for which evaluation for a source of occult infection in a non-toxic child is considered, though some literature report temperatures ≥ 39.5°C as the threshold. It is important to elicit whether these children have any underlying medical conditions that would increase their risk of serious infection such as sickle cell disease or urinary tract reflux. An immunization history is also important in this age group due to the fact that children who have not received 3 doses of the Haemophlius influenza type b vaccine and pneumococcal vaccine are at increased risk for bacteremia in comparison to children who have received all of their immunizations. Other risk factors for occult bacteremia include fever ≥ 39°C and white blood cells (WBC) > 15 000/ μL.
Serious bacterial infections that occur in this age group include meningitis, pneumonia, focal skin infections and osteomyelitis. Pneumonia and urinary tract infections are common causes of occult bacterial infections. Interestingly, the duration of the fever appears to be a poor predictor of bacteremia.
Children between the ages of 3 and 36 months who appear ill or have unstable vital signs should have a septic evaluation including CBC with differential, blood cultures, urine cultures and CSF cultures if meningitis is suspected. A chest radiograph should be ordered for children with respiratory distress, tachypnea, oxygen saturation < 97% or WBC > 20 000. In these cases, empiric antibiotic treatment should be initiated.
Well-appearing children 3 to 36 months of age who have no identifiable source of infection after history and complete physical including examination of the skin, bone palpation and joint range of motion, should be further evaluated. Any child younger than 36 months who has not been fully immunized and infants 6 months of age or younger appear to be at greater risk for bacteremia. Thus, these children should receive a CBC with differential and urinalysis with urine culture completed:
- Children with WBC ≥15 000/μL should receive a blood culture and a strong consideration for parenteral antibiotics.
- Children with WBC ≥ 20 000/μL should have a chest radiograph performed (high probability of occult pneumonia)
- Children should be treated for a urinary tract infection if they have an abnormal urinalysis
Children over the age of 6 months who present with fever, appear well and have received their Hib and pneumococcal vaccinations should have some evaluation. It is recommended that girls younger than 24 months of age and uncircumcised boys younger than 12 months should receive a clean catch or catheter sample urinalysis and urine culture and be treated if the results are abnormal. For girls 24 months and older, uncircumcised boys older than 12 months and circumcised boys older than 6 months routine laboratory investigation and empiric antibiotics are not recommended.
It is very important that follow-up within 24 hours be arranged for those children aged 3-36 months who received antibiotics and within 48 hours for all children with continual fever. Children should also return if their condition further deteriorates or if a positive culture is discovered. It is recommended that positive urine cultures be treated with oral antibiotics and positive blood cultures be treated with parenteral antibiotics and should be admitted to hospital.
Conclusion
Children may present with fever as their only sign of illness. It is your job to determine whether this fever is caused by a serious infection and warrants further evaluation. Literature has provided some guidelines for infants presenting with fever but a thorough history and physical exam is always essential to come up with a source for the infection. Finally, you must always ensure adequate follow up of your patients.
Appendix
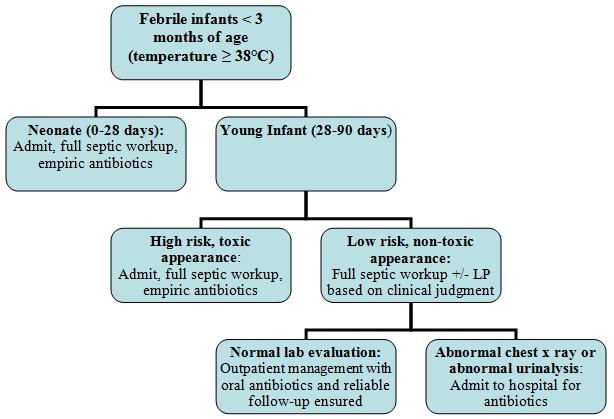
Figure 1: Approach to fever in infants < 3 months of age. Adapted from Kourtis et al, Clinical Pediatrics 2004.
Notes: Full septic workup = blood culture and sensitivity, CBC with differential, urine routine and microscopy, urine culture and sensitivity, lumbar puncture, chest radiograph if respiratory signs and symptoms and stool culture and sensitivity if gastrointestinal signs and symptoms.
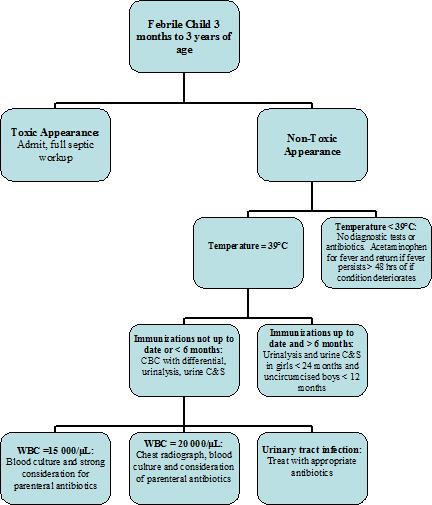
Figure 2: Approach to fever in a previously health child between 3 and 36 months of age. Adapted from Baraff LJ, Annals of Emergency Medicine 2000.
Notes: Urine C&S = Urine culture and sensitivity
References
- Allen, CH. Fever without a source in children 3-36 months of age. Up to Date 2007.
- Baraff, LJ. Management of Fever Without Source in Infants and Children. Annals of Emergency Medicine 2000; 36 (6): 602-614.
- Kleigman RM, Marcdante KJ, Jensen HB, Behrman RE. Nelson Essentials of Pediatrics 5th Edition. Elselvier Saunders, 2006.
- Kourtis AP, Sullivan DT, and Sathian U. Practice Guidelines for the Management of Febrile Infants Less Than 90 Days of Age at the Ambulatory Network of a Large Pediatric Health Care System in the United States: Summary of New Evidence. Clinical Pediatrics 2004; 43: 11-16
- Palazzi DL, Feigin RD. Approach to the child with fever of unknown origin. Up to Date 2007.
- Smitherman HF, Macias CG. Definition and etiology of fever in neonates and infants (less than 3 months of age). Up to Date 2007.
- Smitherman HF, Macias CG. Evaluation and management of fever in the neonate and young infant (less than 3 months of age). Up to Date 2007.
- Smitherman HF, Macias CG. Strategies for the evaluation of fever in neonates and infants (less than 3 months of age) Up to Date 2007.
Acknowledgements
Written by Anne Marie Jekyll
Edited by Jeff Bishop


 (28 votes, average: 4.21 out of 5, rated)
(28 votes, average: 4.21 out of 5, rated)