Click for pdf: Abnormal hip exam
Background
Routine neonatal screening for developmental dysplasia of the hip (DDH) is very important in all newborns. DDH refers to abnormal development of the hip where there is instability (dislocatability) of the hip and dysplasia (abnormal shape) of the acetabulum. Physical examination using the Barlow and Ortolani tests are frequently positive in individuals with DDH, however it is not pathognomonic for dysplasia/dislocation of the femoral head in the acetabulum. Rather, the presence of an abnormal physical exam warrants immediate further investigation and possible intervention. This article outlines the epidemiology, risk factors, signs and symptoms, diagnosis, and treatment of DDH as well as its complications and differential diagnoses.
Epidemiology and Risk Factors
DDH affects one in one thousand live birthsand most commonly in occurs in otherwise healthy infants. Laxity of the hip and immaturity of the development of the acetabulum is often detected in normal newborns in the first few weeks of life. This laxity resolves in most cases and acetabulum goes on to develop normally. The cause of DDH in most cases is unknown, but presumed to be multifactorial despite many competing theories that attempt to explain its etiology.
DDH can however occur in association with other conditions such as Ehlers-Danlos, Down Syndrome and various forms of neuromuscular hip dysplasia. Other causes of DDH are by teratogens during the gestational period.
Risk factors for DDH include female gender, breech presentation, and a positive family history of DDH. Girls with a breech presentation are at the highest risk with an estimated risk of 12%. Boys with a breech presentation have a 2.6% risk. Girls with a positive family history have a risk of 4.4% while boys with a family history of DDH have a risk of only 0.9%. The estimated risk of DDH in girls without other risk factors is 1.9%.
Presentation
Congenital DDH presents along a spectrum that can be classified as: acetabular dysplasia (no dislocation), subluxation or partial dislocation of the femoral head, or complete dislocation of the femoral head from the acetabulum. The clinical presentation of DDH depends upon the age at presentation and the severity of the abnormality (See Table 1). Age at presentation, however, carries the largest impact on treatment options, remodeling ability, and thus final outcome.
Infants with DDH may be asymptomatic or symptomatic. In decreasing frequency, patients present with pathology in the left hip, bilateral hips, and right hip.
|
Age at Presentation |
Clinical Features |
|
Birth to 3 months |
Diagnostic: Hip instability demonstrated by positive Ortolani or Barlow testsSuggestive: Asymmetric leg creases (inguinal, gluteal, thigh, popliteal), apparent shortening of the femur
Associated findings: metatarsus adductus, clubfoot, torticollis, plagiocephaly, extension contractures of the knee |
|
3 to 12 months |
Limitation of hip abduction in 90° of flexionApparent shortening of femurLaterally rotated posture of lower limbsMarked asymmetry of leg creases |
|
After the child begins to walk |
Excessive lumbar lordosisProminent greater trochanterGluteus medius lurchPositive Trendelenburg sign
Short leg limp, with toe-heel gait and out-toeing Increasing adduction contracture of the hip |
Table 1: Clinical Findings in DDH – Adapted from Clinical Features and Diagnosis of DDH, www.uptodate.com
The differential diagnosis of hip instability in the infant includes proximal femoral focal deficiency, congenital coxa vera, infected hip leading to pathologic dislocation, muscle imbalance in children with cerebral palsy or myelomeningocele.
Physical Examination
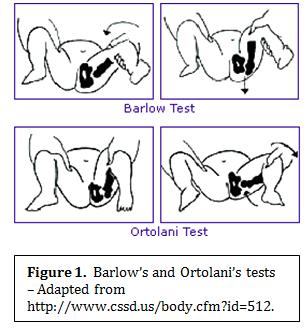
Routine screening for hip dysplasia is performed on all newborns and infants with the Ortolani and Barlow maneuvers. Each hip should be examined separately and ideally when the infant is calm. Place the infant supine with the hip flexed to 90° in a neutral position.
Barlow Maneuver: This test attempts to detect joint subluxation or dislocation by trying to displace the femoral head posteriolaterally from the acetabulum. Place your index and middle finger along the greater trochanter and your thumb on the inner thigh. Then gently adduct the hip and apply pressure posteriorly. You may feel a “clunk” or “jerk” and posterior movement if the hip is dislocatable. You are in feeling the femoral head dislocate out of the acetabulum and this constitutes a positive Barlow test. If the hip is subluxed, you may feel a sliding motion.
Ortolani’s Test: This test attempts to determine if a subluxed or dislocated hip joint is reducible after the Barlow maneuver has been performed. With your hands in the same position as before, gently abduct the hip while lifting the leg anteriorly in an attempt to lift the head of the femur back into the acetabulum. If a palpable “clunk” is detected, this indicates a reducible dislocation and a positive Ortolani’s test.
Note, it is quite common to detect high pitched “pops” or “clicks” without any detection of hip movement or a palpable clunk; these sounds are NOT associated with DDH.
Procedures for Investigation
Radiolographic Evaluation:
Ultrasound is widely used to confirm the diagnosis of DDH and is used to assess the morphology and stability of the hip. It is a useful adjunct until 3 to 5 months of age. However, accurate interpretation requires experience and over reporting is common (25/1000), thus leading to unnecessary treatment in many patients.
X-rays are indicated and more valuable in older infants (>6 months old) and children due to the presence of a greater amount of ossification. It may also be of limited utility in younger infants even if it is coupled with a thorough history and a carefully performed physical exam. An AP radiograph should be obtained with hips in the neutral position; if they are obtained in the newborn period, the hips should be placed at 20-30° A diagnosis on X-ray is made after Hilgeureiner’s (H; horizontal) and Perkin’s (P; vertical) lines have been drawn and the proximal femoral epiphysis is seen to have lateral or proximal displacement, indicating dislocation. If the acetabular index (theta) is measured to be greater than 30 degrees, abnormal acetabular development is probable as shown in figure 2.
Figure 2
Management
Management of DDH varies by age but treatment becomes increasingly difficult with older patients. Any infant with hip instability should be referred to a pediatric orthopedic surgeon.
0-18 months (Dislocated, reducible hip): Neonates with confirmed dislocatable and reducible hip are treated with abduction splinting (Pavlik harness) until stability is confirmed. Infants are not to flex and abduct their hip to greater than 60 degrees to avoid interfering with the blood supply to the femoral head and injury to the femoral nerve.
0-18 months (Dislocated, non-reducible hip): Closed reduction is often possible followed by a spica cast in order to maintain reduction. If closed reduction cannot be done, open reduction is required. This is followed by an arthrography and a CT scan to confirm successful reduction.
18 months – 4 years old: Open reduction is often required. If reduction is well maintained until age 4 the results are good since acetabular remodeling occurs up to 4 years of age.
>4 years old: Treatment is most difficult at this age since acetabular remodeling is minimal. Even a successful reduction may not confer a stable, pain-free hip therefore salvage osteotomies are sometimes performed to improve joint mechanics. In many cases, despite the intervention, a total hip arthroplasty will still be required due to ensuing pain and limited range of motion that many patients experience.
Complications
Avascular necrosis of the femoral head following operative and non-operative treatment is a major complication. Many patients may also experience limited range of motion, and an inability to gain or maintain stable reduction.
Conclusion
The natural history of untreated DDH carries significant morbidity that can be avoided with early intervention. Thus it is extremely important that the hip examination is completed on all newborns as part of the routine newborn assessment.
References
1. Srinivasan Ramesh C, Tolhurst Stephen, Vanderhave Kelly L, “Chapter 40. Orthopedic Surgery” (Chapter). Doherty GM: CURRENT Diagnosis & Treatment: Surgery, 13e: http://www.accessmedicine.com/content.aspx?aID=5314010.
2. Beaty James, “Chapter 27 – Congenital and Developmental Anomalies of the Hip and Pelvis” (Chapter). Canale & Beaty: Campbell’s Operative Orthopaedics, 11th e: http://www.mdconsult.com.ezproxy.library.ubc.ca/books/page.do?sid=1100205994&eid=4-u1.0-B978-0-323-03329-9..50030-1&isbn=978-0-323-03329-9&type=bookPage§ionEid=4-u1.0-B978-0-323-03329-9..50030-1–cesec1&uniqId=231509832-13
3. Nemours Foundation, “Developmental Dysplasia of the Hip”. http://kidshealth.org/parent/medical/bones/ddh.html
4. Lehmann HP, Hinton R, Morello P, et al: Developmental dysplasia of the hip practice guideline: technical report. Committee on Quality Improvement and Subcommittee on Developmental Dysplasia of the Hip. Pediatrics 2000; 105:E57
5. MacEwen GD, Ramsey PL: The hip. In: Lovell WW, Winter RB, ed. Pediatric orthopaedics, Philadelphia: Lippincott; 1978.
6. Medline Plus, “Developmental Dysplasia of the Hip”. http://www.nlm.nih.gov/medlineplus/ency/article/000971.htm
7. Waanders, NA. Clinical features and diagnosis of developmental dysplasia of the hip. UpToDate 2011. www.uptodate.com.
Acknowledgements
Written by: Jacqueline Li
Edited by: Anne Marie Jekyll, MD (Pediatric Resident)




 (10 votes, average: 3.90 out of 5)
(10 votes, average: 3.90 out of 5)