Click for pdf: Approach to Lymphadenopathy
Definition
Lymphadenopathy is defined as enlargement of lymph nodes. This process is often secondary to infection and is frequently benign and self-limited. Viral or bacterial infections lead to localized responses from lymphocytes and macrophages, leading to enlargement of nodes. There may also be localized infiltration by inflammatory cells in response to an infection of the nodes themselves. This is known as a lymphadenitis. Finally, it is crucial to rule out rarer, more serious causes such as lymphomas or leukemias, which are due to proliferation of neoplastic lymphocytes or macrophages.
Normally, lymphoid tissue enlarges until puberty and then undergoes gradual atrophy throughout the rest of life. Normal lymph nodes are most prominent in children ages 4 to 8 years old.
History
Lymphadenopathy is most common in young children whose naïve immune systems respond more frequently to newly encountered infections. There are many different causes of lymphadenopathy, and thus, a thorough history and physical are critical in establishing a diagnosis. It is especially important to rule out possible neoplasms. Some questions that will help narrow the differential include:
- Characteristics of the lymph node(s). Onset, size, duration? Is it painful or erythematous? Generalized or local? Associated symptoms?
- Recent infections. Has this child had a recent infection that may explain a lymphadenopathy? Upper respiratory tract symptoms? Any respiratory symptoms? Rashes? Changes in bowel movements or voiding patterns? Any bone or joint pain? Changes in vision? Headaches?
- Constitutional symptoms? Fever, night sweats, weight loss?
- Skin lesions or trauma? Cat scratch? Animal/insect bites? Other open wounds? Dental abscesses?
- General health. Has this child been hospitalized in the past? Any ongoing medical conditions? Any surgeries? Any visits to the Emergency department?
- Recent Travel & Exposures. Could the child have picked up an infection while traveling? Has the child been in contact with infected individuals? Viral respiratory exposures such as EBV/CMV? TB exposure?
- Immunization status. MMR?
- Medications. Carbemazepine or phenytoin? There are a wide variety of medications which can cause lymphadenopathy.
- Allergies.
- In adolescents, it is also important to ask about IV drug use and obtain a sexual history.
- Cats. Think of toxoplasmosis and bartonella
- Food. Ingestion of unpasteurized animal milk (brucellosis), or undercooked meats (toxoplasmosis, tularemia)
Physical exam
Children often have easily palpable nodes enlarged in response to infection. Nodes that are usually palpable include anterior cervical, inguinal, and axillary regions until about age 12. Palpable nodes in the supraclavicular region are often associated with malignancy of the chest or abdomen and always require further investigation.
Always perform a complete physical exam beginning with general appearance, vital signs and growth parameters. Are they febrile? Plot them on the appropriate growth chart; have they lost weight? Then perform a complete systematic physical exam paying special attention to your head and neck, abdominal and dermatological examinations. Always pay special attention to the area of the enlarged node for a focus of infection. For example, in a child with cervical adenopathy one should examine the orpharynx and consider the possibility of streptococcal pharyngitis or viral upper respiratory infection. Ask if the patient has had a sore throat or ear pain. In an infant with occipital lymphadenopathy, one should examine the scalp for lesions such as seborrheic dermatitis.
Head and Neck – Examine closely for:
– Scalp infection (e.g. seborrheic dermatitis, tinea capitius)
– Conjunctivitis injection
– Oropharynx for pharyngitis, dental problems, HSV ginivostomatitis
– Ears for acute otitis media
Abdomen – Examine closely for:
– Hepatosplenomegaly (this is actually considered part of your lymph node exam!)
– Abdominal masses (e.g. neuroblastoma)
Skin – Examine closely for:
– Any rashes
– Petechiae, purpura, eccyhmoses (e.g. thrombocytopenia)
Lymph Node Exam:
When palpating a lymph node it is important to consider the following:
– Size (measure them)
– Location
– Fixation
– Consistency
– Tenderness
| Less concerning findings | Worrisome findings which increase risk of malignancy |
|
|
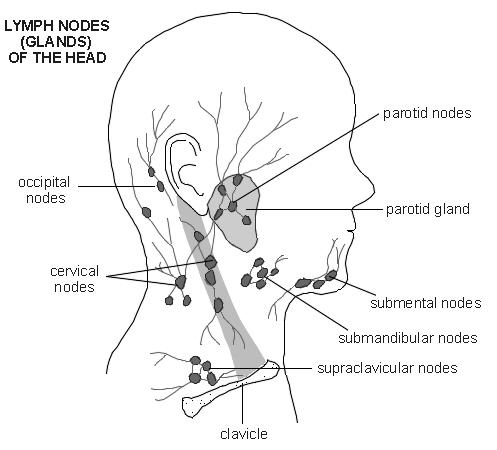
Be sure to examine all the lymph nodes: Pre-auricular, post-auricular, tonsillar, submental, submandibular, anterior cervical, posterior cervical, occipital, supraclavicular, axillary, epitrochlear (in the antecubital fossa), inguinal, popliteal and don’t forget the liver and spleen!!
Figure 1: “Diagram (c)EMIS 2011, as distributed at http://www.patient.co.uk/diagram/Lymph-nodes-head-and-neck.htm, used with permission.”
A careful history and physical exam will help determine whether further investigation is needed.
Differential diagnosis
|
Generalized enlargement of more than 2 noncontiguous lymph node groups |
|
Infectious · Viral (most common): URTI, measles, varicella, rubella, hepatitis, HIV, EBV, CMV, adenovirus · Bacterial: syphilis, brucellosis, tuberculosis, typhoid fever, septicemia · Fungal: histoplasmosis, coccidioidomycosis · Protozoal: toxoplasmosis Non-infectious inflammatory diseases · Rheumatologic diseases: Sarcoidosis, rheumatoid arthritis, SLE · Storage diseases: Neimenn-Pick disease, Gaucher disease · Serum sickness · Rosai-Dorfman disease Malignant: leukemia, lymphoma, neuroblastoma Drug reaction: phenytoin, allopurinol Hyperthyroidism |
|
Localized enlargement of a single node or multiple contiguous nodal regions |
|
A. Cervical (most common adenopathy in children, often infectious cause): Infectious: 1. Viral upper respiratory infection 2. Infectious mononucleosis (EBV, CMV) 3. Group A Streptococcal pharyngitis 4. Acute bacterial lymphadenitis (e.g staphylococcus aureus) 5. Kawasaki disease (unilateral cervical lymph node > 1.5 cm) 6. Rubella 7. Catscratch disease 8. Toxoplasmosis 9. Tuberculosis, atypical mycobacteria Neoplastic: (malignant childhood tumours develop in the head and neck in ¼ of cases. Neuroblastoma, leukemia, non-Hodgkins, and rhabdomyosarcoma are most common in those < 6 years old. In older children, Hodgkin’s and non-Hodgkin’s lymphoma are more common. 1. Acute leukemia 2. Lymphoma 3. Neuroblastoma 4. Rhabdomyosarcoma
B. Submaxillary and submental 1. Oral and dental infections 2. Acute lymphadenitis
C. Occipital 1. Pediculosis capitis (lice) 2. Tinea capitis/local skin infection 3. Rubella 4. Roseola
D. Preauricular (rarely palpable in children) 1. Local skin infection 2. Chronic ophthalmic infection
E. Mediastinal (not directly palpable; assess indirectly via presence of supraclavicular adenopathy. May manifest as cough, dysphagia, hemoptysis, or SVC syndrome – this is a medical emergency!) 1. ALL 2. Lymphoma 3. Sarcoidosis 4. Cystic fibrosis 5. Granulomatous disease (tuberculosis, histoplasmosis, coccidioidomycosis)
F. Supraclavicular (associated with serious underlying disease) 1. Lymphoma 2. Tuberculosis 3. Histoplasmosis 4. Coccidioidomycosis
G. Axillary 1. Local infection 2. Cat scratch disease 3. Brucellosis 4. Reactions to immunizations 5. Non Hodgkin lymphoma 6. Juvenile rheumatoid arthritis 7. Hidradenitis suppurativa
H. Abdominal (may manifest as abdominal pain, backache, urinary frequency, constipation, or intestinal obstruction due to intussuception) 1. Acute mesenteric adenitis 2. Lymphoma
I. Inguinal 1. Local infection 2. Diaper dermatitis 3. Syphilis |
Investigations
- Complete blood count, peripheral blood smear
- Erythrocyte sedimentation rate (non-specific)
- Rule out infectious causes: Monospot, CMV, EBV, & toxoplasma, bartonella titres, TB skin test, Anti-HIV test, CRP, ESR
- Hepatic and renal function + urinalysis (systemic disorders that can cause lymphadenopathy)
- Lactate dehydrogenase, uric acid, calcium, phosphate, magnesium if malignancy suspected
- Bone marrow, liver biopsies, CT or US guided lymph node biopsy
Imaging Studies
- Chest X-ray. This study will help determine the presence of mediastinal adenopathy and underlying pulmonary diseases including tuberculosis, coccidioidomycosis, lymphomas, and neuroblastoma.
- Ultrasound of the lymph node
- CT of the chest and/or abdomen. Supraclavicular adenopathy is highly associated with serious disease in the chest and abdomen.
- Nuclear medicine scanning is helpful in the evaluation of lymphomas.
Management
- Treatment with antibiotics. Bacterial infection results in large nodes that are warm, erythematous, and tender. Start on antibiotics that cover the bacterial pathogens frequently implicated in lymphadenitis, including staphylococcus aureus and streptococcus pyogenes. Reevaluate in 2-4 weeks. Biopsy if unchanged or larger.
- If malignancy is a strong possibility excisional biopsy should be considered immediately.
- If lymphadenitis is present, aspirate may be needed for culture.
Conclusion
In summary, lymphadenopathy is a sign of a variety of underlying disorders, most of which are benign in children. Less commonly, there is a more serious cause of lymphadenopathy and thus it is extremely important to think of and rule out malignancy through a thorough history and physical exam.
References
- McClain, K and Fletcher R. Approach to the child with peripheral lymphadenopathy. UpToDate 2009. www.uptodate.com.
- McClain, K and Fletcher R. Causes of Peripheral lymphadenopathy in children. UpToDate 2009. www.uptodate.com.
- Kleigman RM, Marcdante KJ, Jensen HB, Behrman RE. Nelson Essentials of Pediatrics 5th Edition. Elselvier Saunders, 2006.
Acknowledgements
Writer: Tram Nguyen
Edited: Anne Marie Jekyll


 (107 votes, average: 4.09 out of 5)
(107 votes, average: 4.09 out of 5)