Click for pdf: Otalgia
Background
Definitions
Otalgia: earache or ear pain
Primary Otalgia: ear pain coming from the external, middle or inner ear
Secondary Otalgia: referred pain to the ear
Anatomy and Physiology
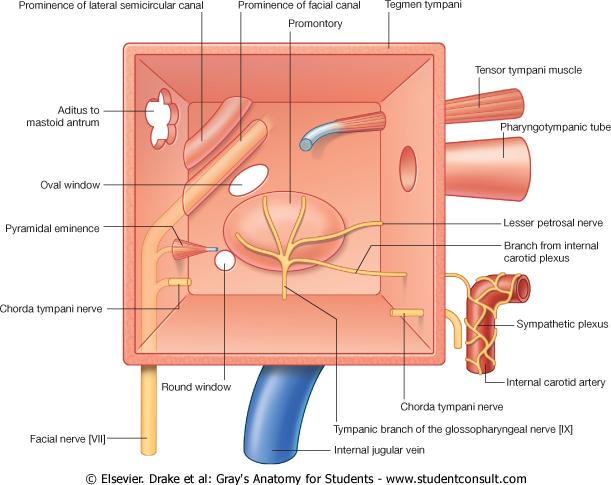
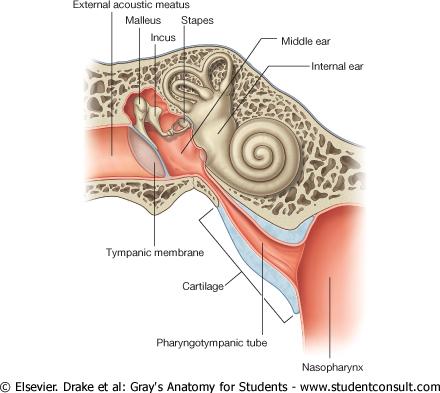
The most common presentation of otalgia is localized to pathology within or around the auricle and a physical examination will uncover the source. Appreciation of the anatomy of the ear will help in the examination but more importantly, it will help in diagnosing when no identifiable pathology is found on examination. The trigeminal, facial, glossopharyngeal, vagal and C2/C3 send sensory afferents to the middle ear, external ear, auricle and periauricluar area; consequently, pain referred via these nerves can cause otalgia.
Figure 1: Journey of the facial nerve and branches of the facial and glossopharyngeal nerve through the middle ear. (Adapted from (1))
Figure 2: Internal structure of the ear. (Adapted from (1))
Historical investigation
A careful history can help distinguish various conditions and in combination with a careful physical exam should provide enough information to make a diagnosis. In infants, the only possible clue of ear pain maybe ear pulling or rubbing in conjunction with irritability, poor sleep or fever.
If the child is able to answer questions, the timing and severity of the pain can help in the differential.
Severe pain: acute otitis media, otitis externa, TMJ dysfunction (worse with eating)
Intermittent severe pain: Chronic otitis media with effusion (glue ear)
Moderate pain: referred pain
Furthermore, it’s important to enquire the patient or parent about purulent otorrhea, hearing loss, swelling, nystagmus, tinnitus or facial paralysis
Table 1: History and possible corresponding diagnosis
| History | Possible Diagnosis |
| Purulent Otorrhea | Otitis externa, otitis media with perforation of tympanic membrane, trauma, neoplasm |
| Hearing Loss | Otitis media (most common), Otitis externa |
| Swelling | Otitis externa, perichondritis, mastoiditis, trauma, benign cystic masses, neoplasms |
| Nystagmus | Vestibular in origin |
| Tinnitus | Eustachian tube – middle ear disease |
| Facial Paralysis | Acute otitis media (most common) |
Physical Examination
A complete examination of the head and neck is warranted when a child presents with otalgia. Many underlying congenital abnormalities can contribute to ear problems like cleft palate and nasopharyngeal tumours which are associated with otitis media.
The ease at which a physical is performed depends on the age and their ability to cooperate.
Position
Child should examined on an examination table or parent’s lap
An assistant or restraint may be necessary to help examine
Examination of the ear
- Inspect auricle and external auditory meatus:
- Inflammation of posterior auricular area may indicate periosteitis or subperiosteal abscess from mastoid cells
- Presence of preauricular pits or skin tags have higher incidence of sensory neural hearing loss (SNHL)
- Inspect the ear canal with otoscope:
- Inflammation of ear canal associated with otitis externa
- Abnormalities of canal like stenosis, bony exostoses, otorrhea can predispose one to otitis externa
- Cholesteatoma of middle ear can display in canal as foul-smelling exudate
- Tympanic membrane (TM) mobility:
- Using pneumatic otoscope, bulging TM caused by increased middle ear air pressure
- Retracted eardrum indicates negative middle ear pressure
- Tympanic membrane appearance:
- Normal appearance is silvery-gray, visualize malleus, incus
- Middle ear effusion – white or yellow
Differential Diagnosis (selected)
Table 2: Common pediatric otalgia differentials (Adapted from (4))
Cause |
Onset |
Character |
Location |
Pattern |
Precipitating factors |
Acute Otitis Media |
Acute | otalgia, decreased hearing, fever | affected ear | persistent otalgia | URTI |
Chronic Otitis Media |
Chronic | recurrent or persistent otorrhea | affected ear | mucopurulent discharge | none relevant |
Otitis Externa |
acute | moderate to severe ear pain and otorrhea | affected ear | persistent otalgia | swimming exposure |
| Eustachian Tube Dysfuncation | chronic | intermittent ear blockage | affected ear. May be bilateral | worse with supine position, increased pressure | none relevant |
Dental Infection |
subacute | dull aching pain in tooth socket | radiates to ear | persistent, worse with eating | poor dental hygiene |
Mastoiditis |
acute | otalgia, decreased hearing, fever | affected ear | persistent or worsening otalgia | antecedent URTI |
| Temporomandibular Joint Syndrome | acute, chronic | mild/severe pain over TMJ | radiates to ear | worse with jaw motion | night time bruxism |
Chickenpox |
acute | otalgia, fever, vesicular skin rash | nonspecific | varying | cluster of infections |
Summary
Most common causes of otalgia will be a local cause, otitis media or externa, but it is important to be suspicious of referred pain to the ear which may indicate a more serious pathology. Treatment varies for the different etiologies of otalgia. For common local infections causing otalgia, it is not uncommon for physicians to restrain from antibiotic use for 3-5 days and observe whether the infection is resolving. A referral to a pediatric otolaryngologist is warranted for any of the causes of otalgia that has not resolved with treatment, especially otalgia resulting in hearing loss.
References
(1) Drake R et al. Gray’s Anatomy for Students. Churchill Livingstone, 2004.
(2) Cummings CW et al. Otolaryngology – Head and Neck Surgery, 4th Edition. Mosby, 2005.
(3) Behrman RE et al. Nelson Essentials of Pediatrics, 17th Edition. Elsevier Saunders, 2004.
(4) Fairchild DG et al. Differential Diagnosis – Ear Pain. FirstCONSULT, Elsevier, 2007.
(5) Corbridge R, Steventon N. ENT and Head and Neck Surgery. Oxford University Press, 2006.
Acknowledgements
Writer: Andrew Thamboo
Editor: Elmine Statham