Click for pdf: Hepatomegaly
General Presentation
Hepatomegaly can represent intrinsic liver disease or may be the presenting physical finding of a generalized disorder. It is important to realize that the liver is easily palpated in most children at 1-2 cm below the right costal margin. A normal liver should feel soft and is easily moveable upon inspiration.
An enlarged liver rarely presents alone and usually accompanies other clinical signs and symptoms based on the underlying pathophysiology. Associated signs and symptoms to watch out for in the pediatric population include shortness of breath, fatigue, abnormal bruising, jaundice, loss of consciousness, seizures, diarrhea, and splenomegaly.
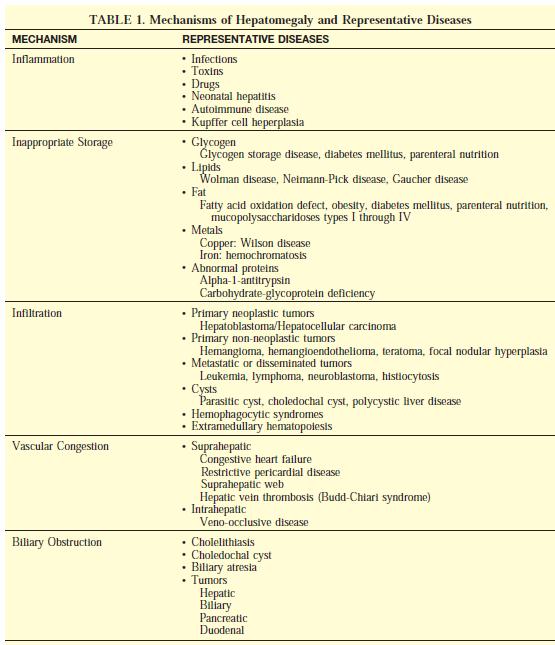
General mechanisms of hepatomegaly include inflammation, excessive storage, infiltration, congestion, and obstruction
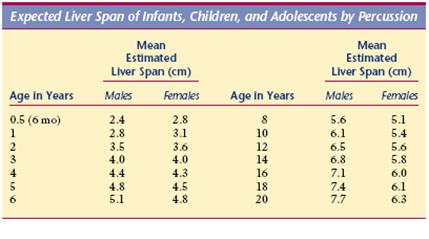
Table 1: Expected liver span in the pediatric population by percussion
(Adapted from Bate’s Guide to Physical Examination and History Taking)
|
Signs of an Abnormal Liver |
|
· >3.5cm below the right costal margin in a newborn · Rubbery (hepatitis) · Tender (acute hepatitis, right heart failure, venous congestion) · Firm (cirrhosis) · Nodular (malignancy) |
Questions to Ask
- Is there any history of recent infection? (eg: rash, pharyngitis, cough, SOB, fever, exposure, poorfeeding, malaise etc)
- Has the child consumed any contaminated food or experienced any diarrhea and/or vomiting?
- Is there any history of loss of consciousness or seizures?
- Does the child have any preexisting liver diseases, lung diseases, or congenital heart diseases?
- Were there any complications during pregnancy, delivery, and after delivery? Are there any growth (weight gain) and developmental concerns?
- Is there any maternal history of hepatitis B or C, CMV, EBV or HIV?
- Is there any family history of cystic fibrosis, alpha-1 antitrypsin deficiency, storage diseases, liver diseases, heart diseases, autoimmune diseases or malignancy?
- Has the child had any change in stool color? What color are his/her stools?
- Is there any history of drug or toxin ingestion? Is there any exposure to radiation?
- Is the child on any medications right now?
- Is there any recent travel?
- Is there any history of trauma?
General Physical examination
- DERM: Petechiae and purpura (malignancy); pruritis/jaundice (liver disease);rashes (infection)
- HEENT: Icterus, cherry red retinal spots or cloudy cornea (lipid storage disease), Kayser-Fleischer (Wilson’s disease)
- CNS: decreased LOC, seizures (hypoglycemia due to storage disease)
- CV/ RESP: Murmur, abnormal heart sounds (S3, S4) (congenital heart diseases), SOB/ abnormal breath sounds (alpha-1 antitrypsin deficiency)
- GI: tenderness, distension, ascites, hepatomegaly (liver disease, gallstones, trauma), splenomegaly (hemolytic anemia)
- MSK: joint tenderness (hepatitis), bone pain (malignancy)
Liver Exam:
Percussion:
- Liver span is determined better by percussion than by palpation in children.
- Percuss along the midclavicular line to find the upper margin of the liver. The transition from resonance to dullness indicates the upper liver border
Palpation:
- Start palpating from the lower right quadrant and work towards the costal margin. Direct fingers inwards upon each inspiration to feel the liver edge.
Scratch test (Figure 1):
- Place the diaphragm of your stethoscope just above the right costal margin at the midclavicular line. Lightly scratch the skin of the abdomen with the fingertip along the midclavicular line, starting from below the umbilicus towards the costal margin. A change in sound indicates the liver edge.
Figure 1. The scratch test to determine the liver’s edge. (Adapted from Bate’s Guide to Physical Examination and History Taking)
Laboratory Investigations
- AST, ALT, GGT, alkaline phosphatase, bilirubin, total protein, albumin
- Serum electrolytes and BUN
- Urinalysis
- CBC with differential and peripheral blood smear
- Fasting blood glucose
- Hepatitis serology
- Additional investigations based on clinical suspicion: EKG, total and direct bilirubin, lipid profile, ceruloplasmin, alpha-1-antitrypsin (AAT), HIV serology, blood culture, autoantibodies, alpha fetoprotein, bone marrow aspiration and biopsy
|
|
Glucose |
Lactate |
Free Fatty Acids |
B-Hydroxybutyrate |
|
Glycogen Storage Diseases |
↓ |
N |
N |
N |
|
Defect in Gluconeogenesis |
↓ |
↑ |
N |
↓/N |
|
Defect in Fatty Acid metabolism |
↓ |
N |
↑ |
↓ |
Table 2: Common laboratory findings in storage diseases that cause hepatomegaly. (Adapted from Sperling Pediatric Endocrinology, 3rd ed.)
Imaging
- Abdominal ultrasound with Doppler
- Abdominal CT or MRI (hepatic masses, biliary tree, anatomical obstructions)
- Echocardiogram (congenital heart defects)
- ERCP (stones)
Liver Biopsy
Conclusion
- Hepatomegaly is a symptom that can be caused by a variety of conditions that affect different organ systems. When evaluating a child with hepatomegaly it is very important to identify conditions in which immediate medication intervention is needed and provide appropriate treatment options.
References
1) McClain K, Landaw S. Approach to the child with an enlarged spleen. (Last updated: July 22, 2008) In: UpToDate, Mahoney D, Hoppin A (Ed), UpToDate, Wellesley, MA, 2010.
2) Anand B, Krok K, Pollak E. Evaluation of hepatomegaly. First Consult (Last updated September 19,2007). Available from: http://www.mdconsult.com [Accessed on January 8, 2010]
3) Bickley L, Szilagyi P, Bates B. Bate’s Guide to Physical Examination and history Taking, 10th ed. Philadelphia: Wolters Kluwer Health/ Lippincott Williams & Wilkins, 2009.
4) De Leon D, Stanely C, Sperling M. Hypoglycemia in Neonates and Infants (Chapter 5). In: Sperling M, editor. Pediatric Endocrinology, 3rd ed. Philidelphia: Saunders, 2008. P 165-197.
5) Kliegman R, Behrman, Jenson H, Stanton B. Nelson Textbook of Pediatrics, 18th ed. Philadelphia: Saunders, 2007.
Acknowledgements
Written by: Leslie Leung
Edited by: Dianna Louie
 |



 (24 votes, average: 4.21 out of 5)
(24 votes, average: 4.21 out of 5)
some truly interesting points you have written.