Click for pdf: ChestPain
General Presentation
In children and adolescents, chest pain is a commonly encountered problem. Despite much concern that underlying cardiac pathology is at play, the percentage of pain attributed to a cardiac etiology is low with an incidence of less than 5%.
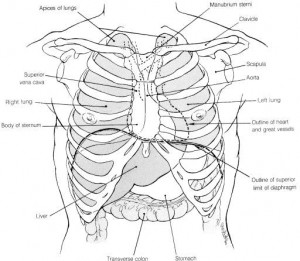
Within the thorax, several organ systems can cause or contribute to pain perceived as coming from the “chest”. The respiratory, cardiovascular, gastrointestinal, musculoskeletal and nervous systems all need to be considered when evaluating the origin of chest pain. Pain from the musculoskeletal system can come from bone, cartilage, muscle, tendons, or ligaments. When attempting to differentiate cardiac from musculoskeletal pain, the key often lies in the history, which is provided by your physical exam.
Figure 1
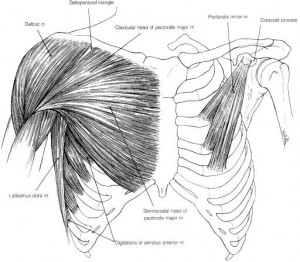
Figure 2
Questions to Ask
- Seek information regarding the quality (sharp, stabbing vs. aching?) of pain, intensity, location (can they point to location with one finger?) and whether it radiates.
- Timing of the pain with relationships to exercise, eating, how long the episodes lasts and how often they occur (duration and frequency helps determine how serious it is, generally if it is brief, infrequent and resolves completely it is less worrisome).
- Ask about any history of trauma.
- How long has it been going on for? If it has persisted longer than several months, a serious organic etiology is unlikely to be the cause.
- What makes it better or worse? In the absence of fever or respiratory symptoms, pain that is worse with inspiration makes the musculoskeletal system more likely.
- Are there any constitutional symptoms (fever, weight loss, fatigue)?
- Are there any respiratory symptoms (e.g. cough, SOB, wheeze)?
- Are there any cardiac symptoms (e.g. palpitations, dizziness, syncope)?
- Are there any GI symptoms or history of GERD (e.g. vomiting, dysphagia, water brash)?
- History of Kawasaki’s disease, rheumatic fever or preceding viral illness?
- What do they think is causing the pain?
- Any recent stressors at home or school or problems with anxiety?
Cardiac vs. MSK type pain
| Cardiac type pain | MSK type pain |
|
|
Differential Diagnosis
- Non Cardiac Causes
- Idiopathic
- Musculoskeletal (chest wall strain, trauma, costochondritis, precordial catch syndrome, slipping rib syndrome)
- Psychogenic
- Respiratory (asthma, pneumonia, pneumothorax, pneumomediastinum)
- Gastrointestinal (GERD, esophagitis, gastritis)
- Miscellaneous (breast mass, sickle cell disease, tumor, herpes zoster)
Cardiac Causes
- Structural (anomalous origin, hypertrophic cardiomyopathy, aortic stenosis
mitral valve prolapse) - Inflammatory (pericarditis, myocarditis)
- Dysrhythmias (SVT, VT)
- Acquired (hyperlipidemia/early coronary artery disease, Kawasaki disease)
- Other (vasospasm, connective tissue disorders)
More about MSK type pain
- Chest wall pain is common in pediatrics. Strains and costochondritis result from overuse. Strains usually involve the major muscle groups of the chest while costochondritis affects one or more of the rib cartilages.
- Precordial catch syndrome causes a sharp, well-localized pain occurring at rest. Typically it lasts seconds to minutes and is aggravated by deep breathing and relieved somewhat by sitting up straight and the physical exam is normal.
- The slipping rib syndrome involves the eighth, ninth, and tenth ribs which are joined together by fibrous tissue. Laxity of the fibrous tissue can cause these ribs to slip over one another. The patient may feel a clicking sensation, followed by a dull ache in either upper abdominal quadrant. During examination, lifting the ribs anteriorly with hooked fingers reproduces the sensation.
Investigations
Physical exam
- A complete general physical exam with vitals (including BP!!!)
- Inspection: you should look for any signs of trauma (bruising, swelling etc.), symmetry of chest wall and sternum
- Palpation: you will want to palpate the thorax for any tenderness, as well feel for any thrills or heaves and feel for distal pulses
- Percussion: if suspect underlying respiratory etiology
- Auscultation: listen to all lung fields and over the four cardiac areas. Listen for S1 and S2, S2 splitting, any S3S4 or murmurs?
- Finally see if you can reproduce the pain by having patient twist, push/pull against resistance, breath deeply, raise arms above head etc. If the history or physical make you concerned about a serious underlying pathology, further tests should be ordered with possible referral to a pediatric cardiologist.
Laboratory investigations
- Chest x-ray: helpful if suspect rib fractures, pneumonia, pneumothorax, cardiac anomalies
- Toxicology screen: cocaine use can cause cardiac ischemia
- Echocardiogram: helpful to detect structural cardiac anomalies
ECG
- Useful in detecting ischemic heart disease
References
Joseph R. Cava, Pamela L. Sayger. Chest pain in children and adolescents. Pediatr Clin N Am 51 (2004) 1553– 1568 (note: figures taken from this journal article)
Jerold C. Woodhead. Pediatric Clerkship Guide. Mosby Inc.2003
Richard E. Behrman, Robert M. Kliegman. Nelson Essentials of Pediatrics. Saunders, Pennsylvania. 2004
Acknowledgments
Written by: Christa McPherson
Edited by: Jeff Bishop


 (8 votes, average: 4.50 out of 5)
(8 votes, average: 4.50 out of 5)
FIVE STARS